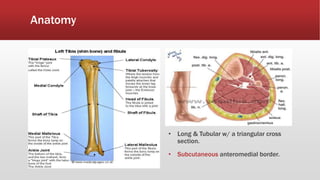
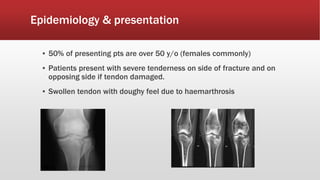
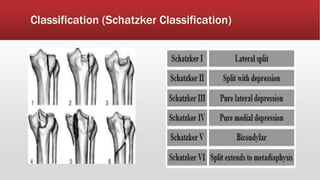
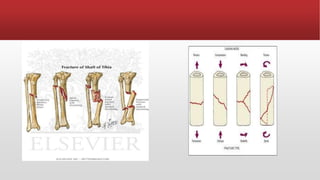
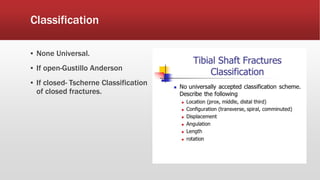
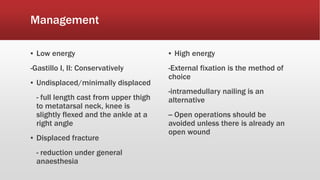
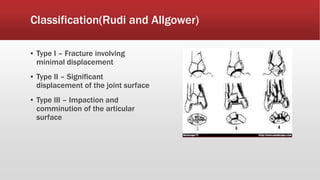
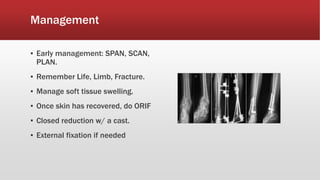
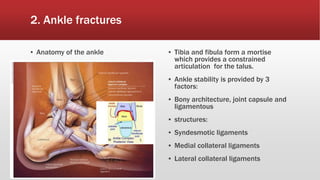
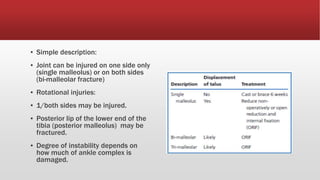
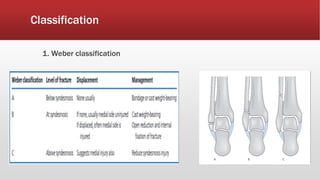
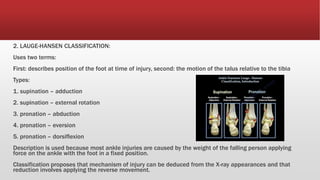
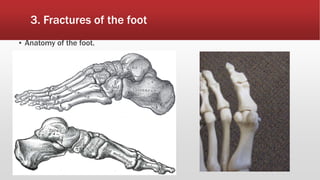
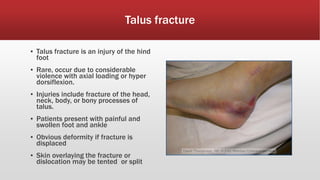
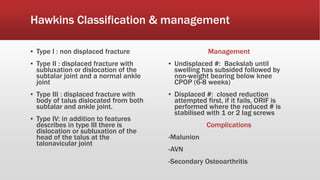
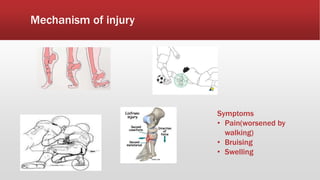
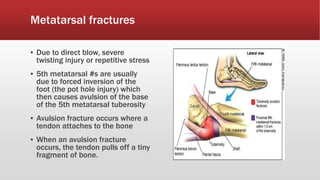
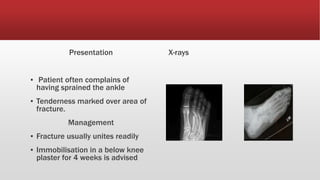
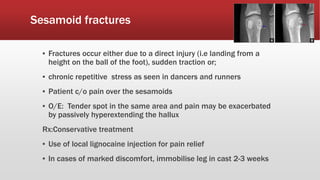
This document provides an overview of lower limb fractures, including fractures of the tibia (proximal, shaft, and distal), ankle, and foot. Key points discussed include the anatomy and mechanisms of injury for each fracture type. Classification systems and approaches to clinical examination, imaging, and management are described. Common complications are also outlined. The level of detail provided is intended for medical students to gain foundational knowledge on evaluating and treating lower limb fractures.