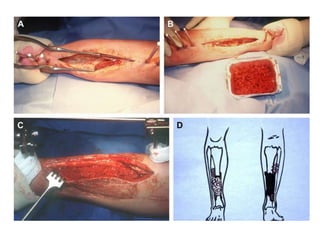
The Masquelet technique is a two-stage process for treating bone defects using an induced membrane. In the first stage, radical debridement is performed followed by insertion of an antibiotic-loaded cement spacer and soft tissue coverage. This induces the formation of a membrane rich in growth factors. In the second stage 6-8 weeks later, the spacer is removed and cancellous bone graft is placed within the membrane chamber, which acts as a bioreactor promoting graft healing. The technique provides an alternative to bone transport or vascularized grafts for reconstructing large defects.