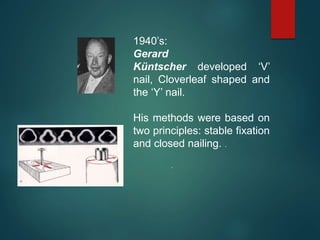
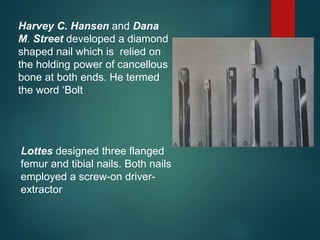
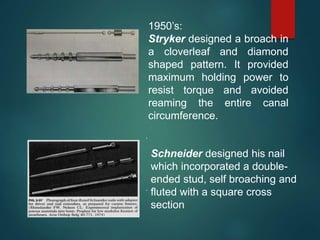
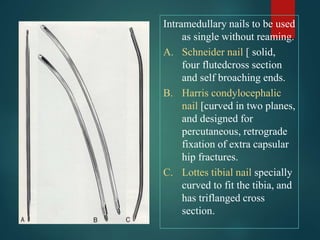
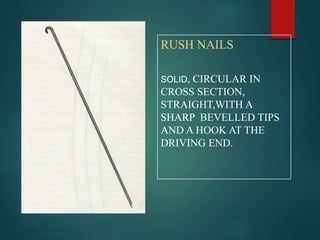
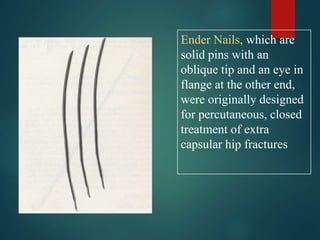
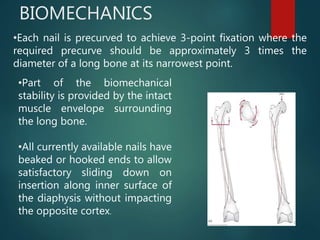
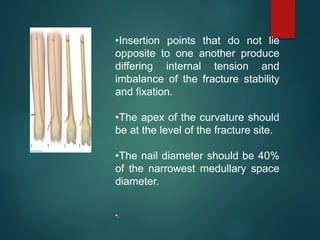
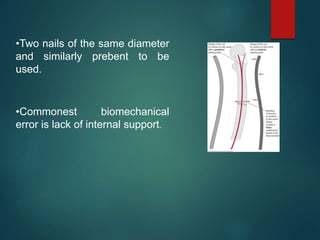
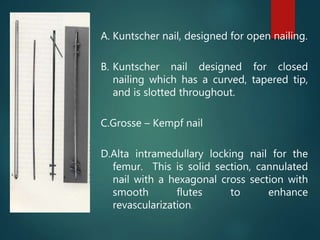
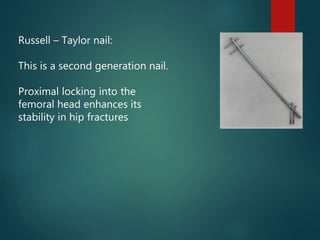
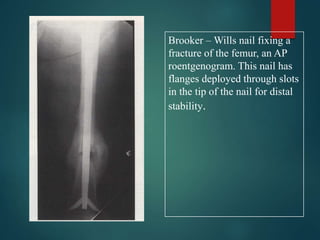
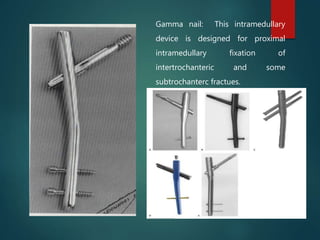
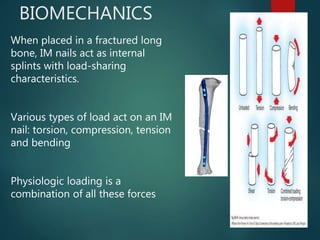
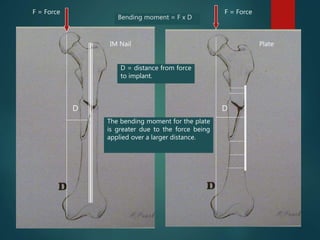
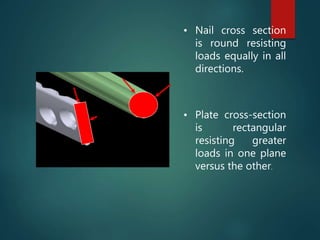
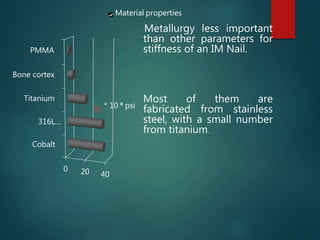
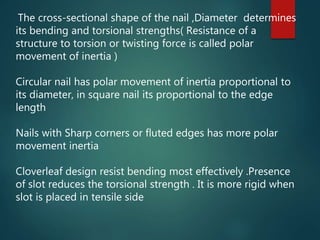
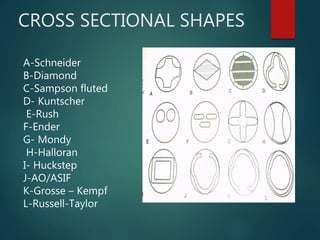
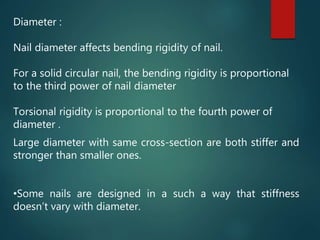
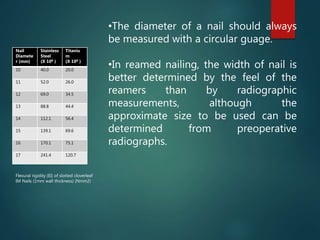
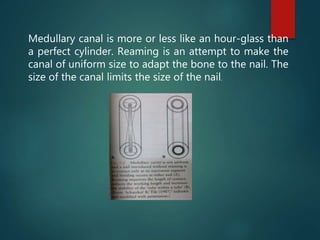
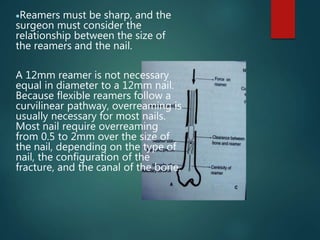
This document provides an overview of intramedullary nailing principles. It discusses the history and evolution of intramedullary nails from wooden sticks and ivory pegs used in the 16th century to modern nails like the Russell-Taylor nail. It covers nail types, biomechanics, insertion techniques, and key design considerations like diameter, cross-section shape, curves, and locking mechanisms. The goal of intramedullary nailing is to provide stable internal splinting of long bone fractures through closed fixation techniques.