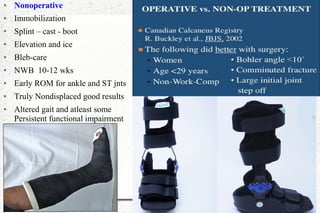
The document discusses calcaneal fractures, covering aspects such as anatomy, mechanisms of injury, classification, diagnosis, treatment, and complications. It highlights the different types of calcaneal fractures, their causes, clinical features, radiological evaluation, and treatment approaches, both operative and non-operative, tailored for various patient demographics including pediatric cases. Additionally, it details complications that can arise from these fractures and their management strategies.
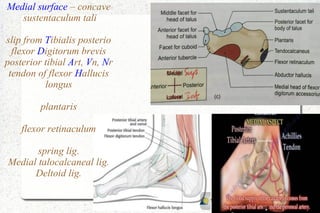
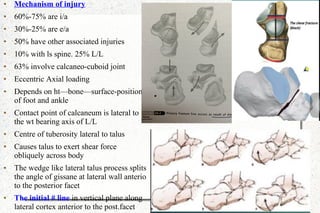
![● The primary # line runs from
portereomedial to anterolateral
calcaneus results into two thalamic
fragments
● The anteromedial/superomedial
/sustentacular/constant fragment
● Attached to deltoid lig. Will move
inferiorly medially and posteriorly
● Posterolateral/superolateral/
semilunar/comet fragment
● Will move superiorly laterally and
anteriorly
● Foot in pronation - #line
posterolateral to post.facet [2A]
● Foot Neutral – # line roughly
through middle of post.facet [2B]
● Foot Supination – # line
anteromedial to post.facet [2C]](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-11-320.jpg)
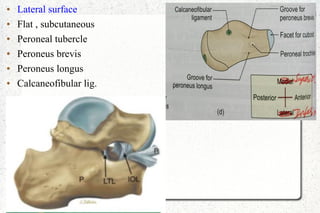
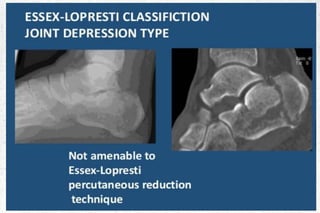
![● Secondary # line
● Exists proximal to tendo
achillies insertion then it is
joint depression type
● Exits distal to tendoachillies
insertion then it is tongue type
● Anteriorly the secondary # line
may extend to calcaneo-cuboid
joint [I/A] or
[E/A] plantar surface , lateral
wall , medial wall](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-12-320.jpg)
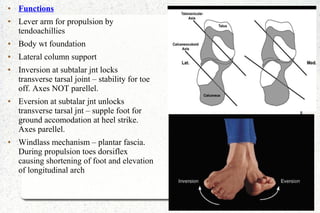
![● Clinical feature
● Pain / tenderness
● Soft tissue injuries
● Skin blisters
● Open # are 7%-17%
● Compartment syndrome
● Skin necrosis at posterior edge
● Thompson test – loss of plantar
flexion with manual calf compression
[tuberosity #]
● Hoffa's sign – laxity of achillies
tendon and weakness of plantar
flexion [I/A #]
● Evaluate comorbidyties to guide Rx
and outcomes --- pvd / dm / smoking /
bmi / age / gender / occupation /
?ambulatory](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-13-320.jpg)

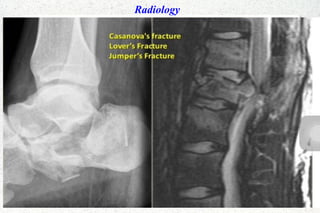
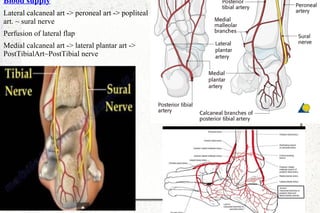
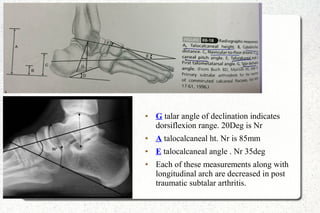
![Xrays – 5 views
● Ap – calcaneocuboid joint
● Obliq – anterior facet and anterior process.
● Lateral- traction & compression trabecula. Neutral triangle . Thalamic portion is
condensed cortical bone inferior to post. Facet.
● Bohler [tuber angle ] normal 20-40 deg. Decreased in ht loss. Corelates with outcome.
● Crucial angle of gissane –Nr is 100 – 120 deg. Relation between 3 facets](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-23-320.jpg)
![TREATMENT● Goals
● Congruency of ST and CC joints
● Restoration of ht [Bohler's angle]
● Reduction of width
● Decompression of subfibular
space for peroneal tendons
● Valgus realignment tuberosity
● Stable fixation
● Timing & important factors
● Age & other injuries
● General health & comorbidity
● Soft tissue envelope – tense
fascia - # blebs
● Open wounds & coverage
● Wrinkle test
● Operative
● Displaced I/A of post.facet
● >25% CC joint involved
● Displaced tuberosity #
● # dislocations
● Open #
● Non-operative
● Mini.displaced E/A
● Undisplaced I/A
● <25% CC joint involved
● Severe pvd
● Household ambulators
● Insulin dependent dm
● Medical comorbidity](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-28-320.jpg)
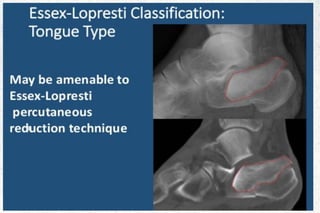
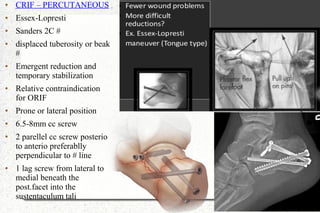
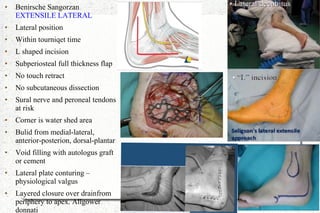
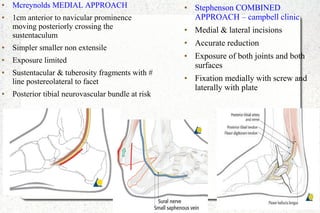
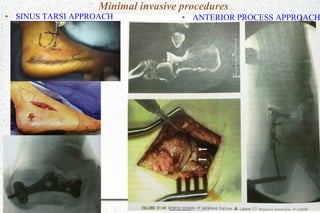
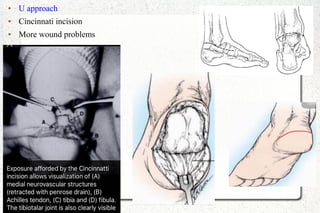
![OPERATIVE
METHODS
● Essex Lopresti CRIF
● Benirsche Sangorzan
EXTENSILE
LATERAL
● Mcreynolds'
MEDIAL
APPROACH
● Stephenson
COMBINED
● U [Cincinnatti]
APPROACH
● ANTERIOR
PROCESS
APPROACH
● Bg Weber TBW
● Carr PRIMARY
ARTHRODESIS](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-30-320.jpg)
![● Carr [gallie's] primary arthrodesis
● Subtalar or triple arthrodesis
● For sanders 4, severe open sander 3.
● Correct any deformities
● Restore calcaneal ht and orientation
● Maintain talar declination angle and
valgus
● Autologus graft placement
● Denude lateral aspect of talus
● 2 large 6.5-8mm cc screwplaced into
corner of heel, perpendicular to
subtalar joint, entering the talus dome.
● Bg Weber tension band wiring
● For tendo achillies avulsions
● Prone position
● May need tendo achillies
lengthening or gastroc resection
● Splint in plantarflexion](https://image.slidesharecdn.com/calcaneum-161020124406/85/Calcaneum-fractures-36-320.jpg)