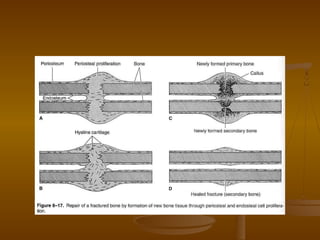
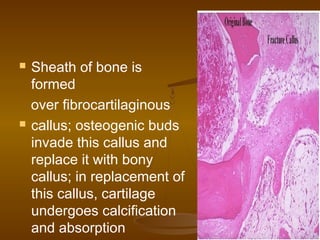
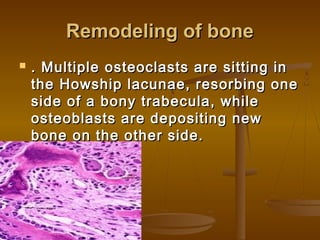
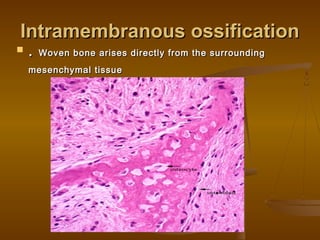
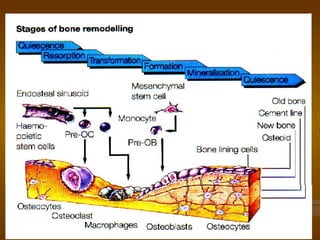
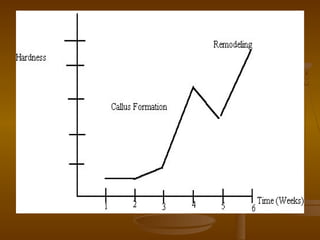
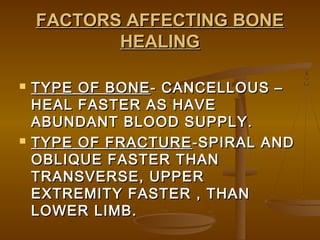
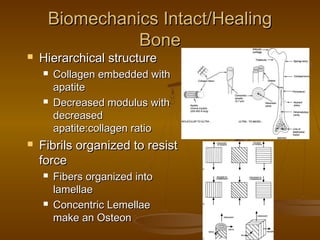
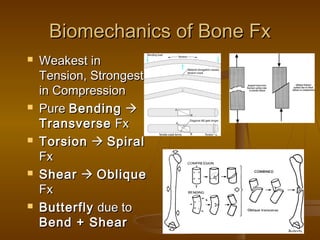
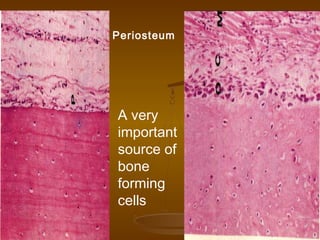
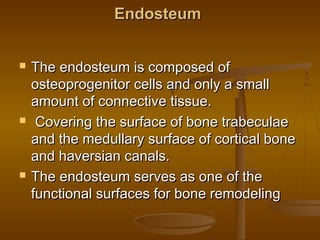
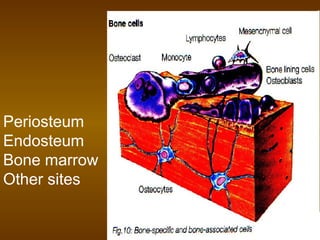
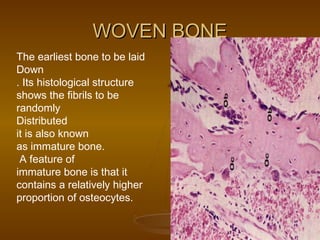
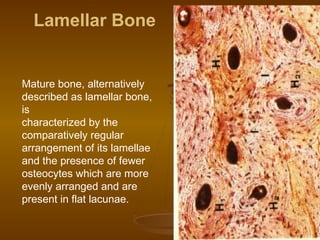
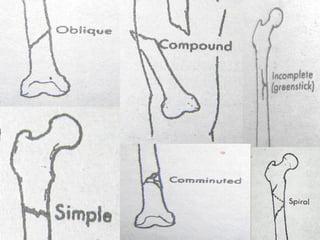
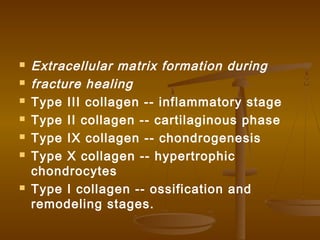
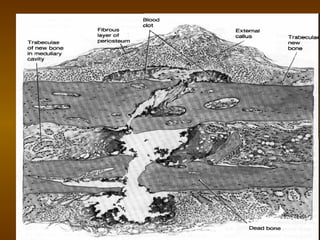
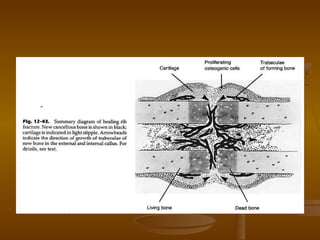
This document discusses bone structure and fracture healing. It describes how bones are composed of minerals and store calcium, phosphate and magnesium. The periosteum and endosteum are important sources of bone forming cells. There are two types of bone tissue - compact bone which is dense and cortical, and sponge bone which is cancellous and located in the marrow cavity. Woven bone is immature bone tissue with randomly arranged collagen fibers, while lamellar bone is mature bone composed of concentric layers. Fractures heal through stimulation of the periosteum and endosteum, which results in new bone formation.

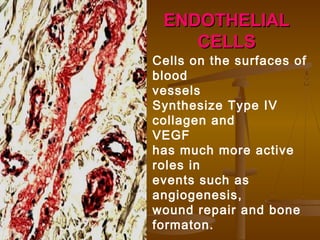




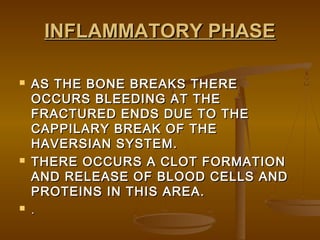
![ Activated platelets release a variety of
products [e.g. Fibronectin; platelet-derived
growth factor (PDGF); transforming growth
factor β (TGF-β)] which trigger the influx of
inflammatory cells. The subsequent cytokine
cascade brings the cells of repair (fibroblasts,
endothelial cells and osteoblasts) into the
fracture gap.](https://image.slidesharecdn.com/fracturesandfracturehealing-170120124005/85/Fractures-and-fracture-healing-88-320.jpg)