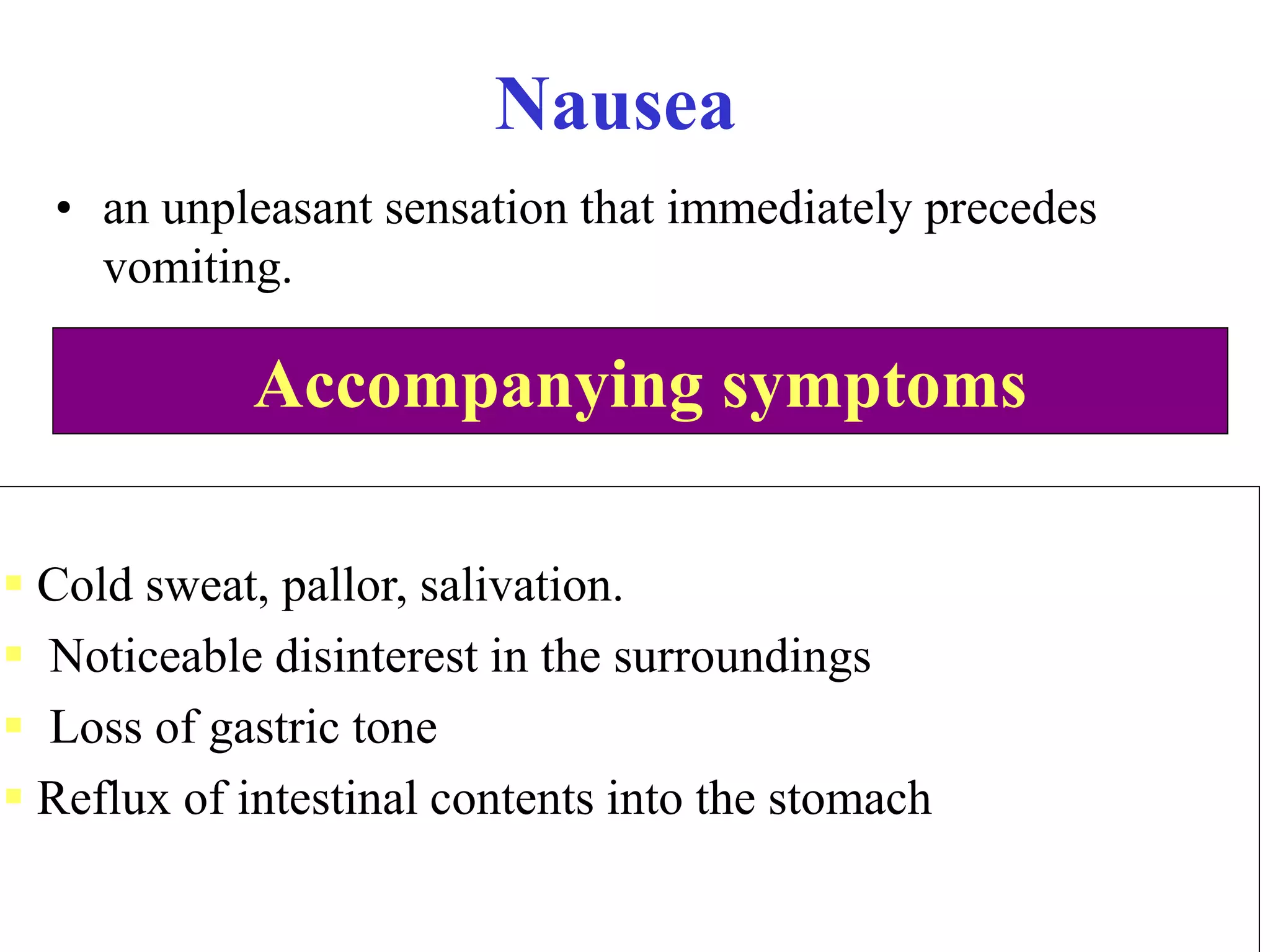
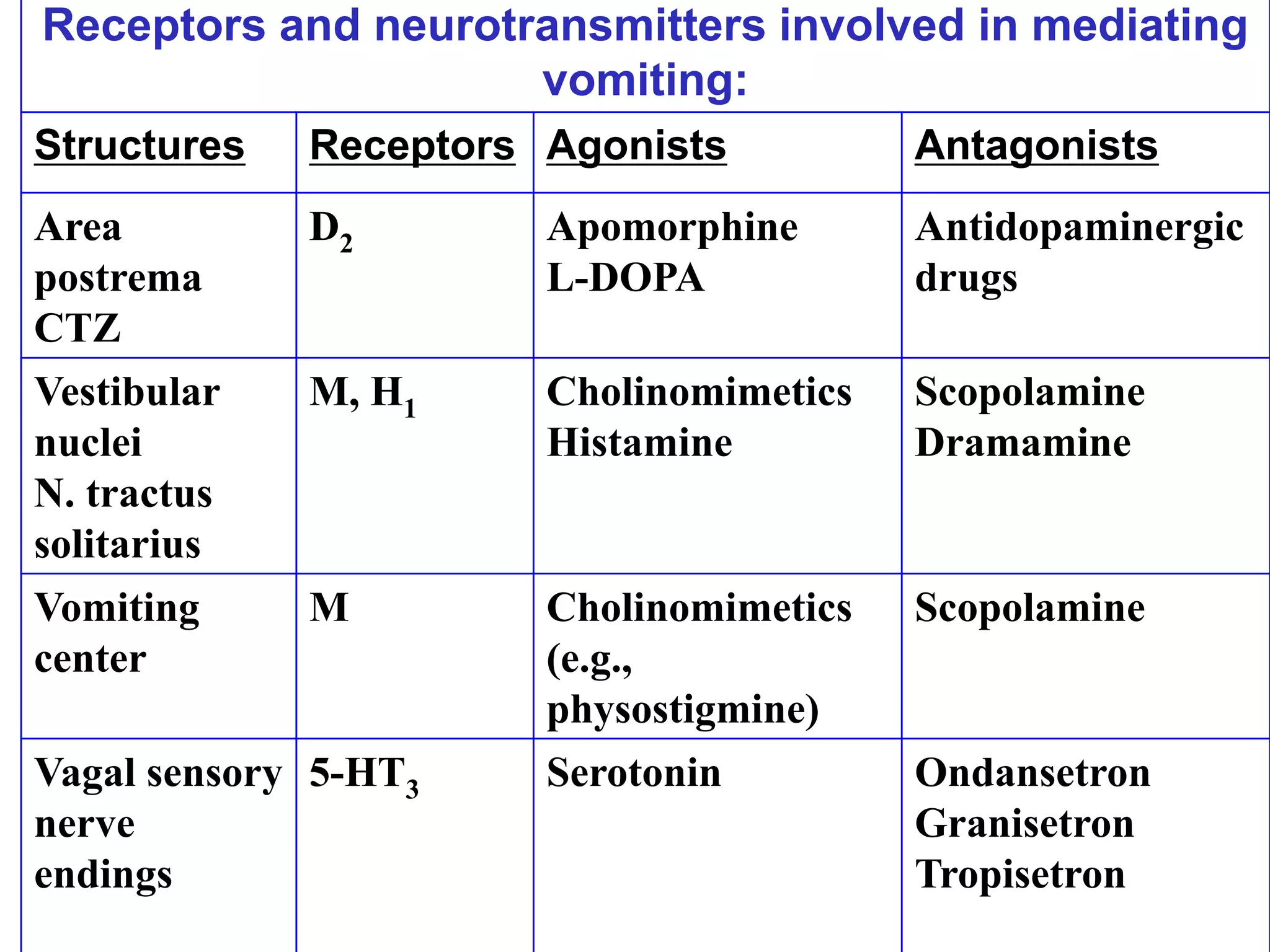
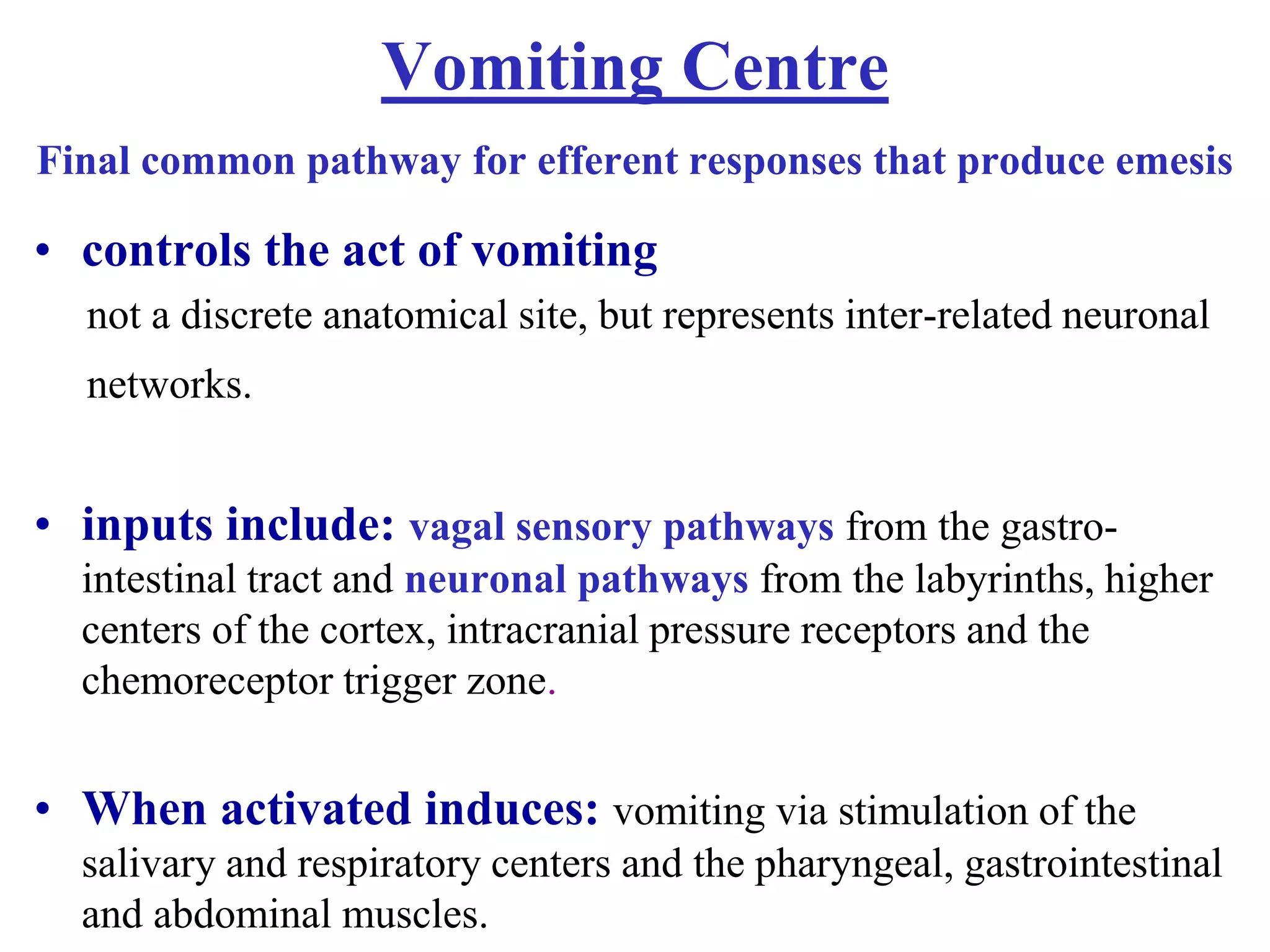
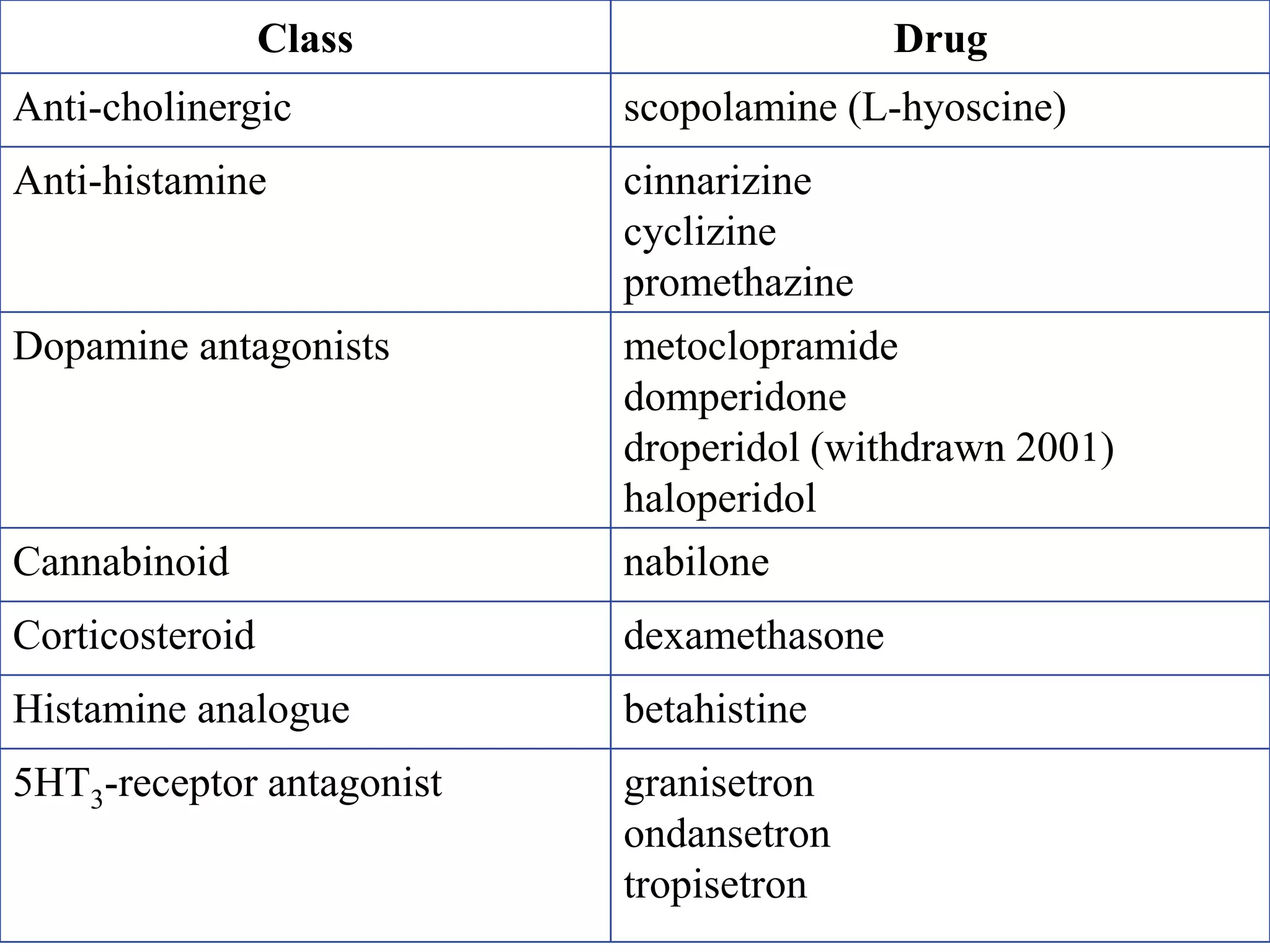
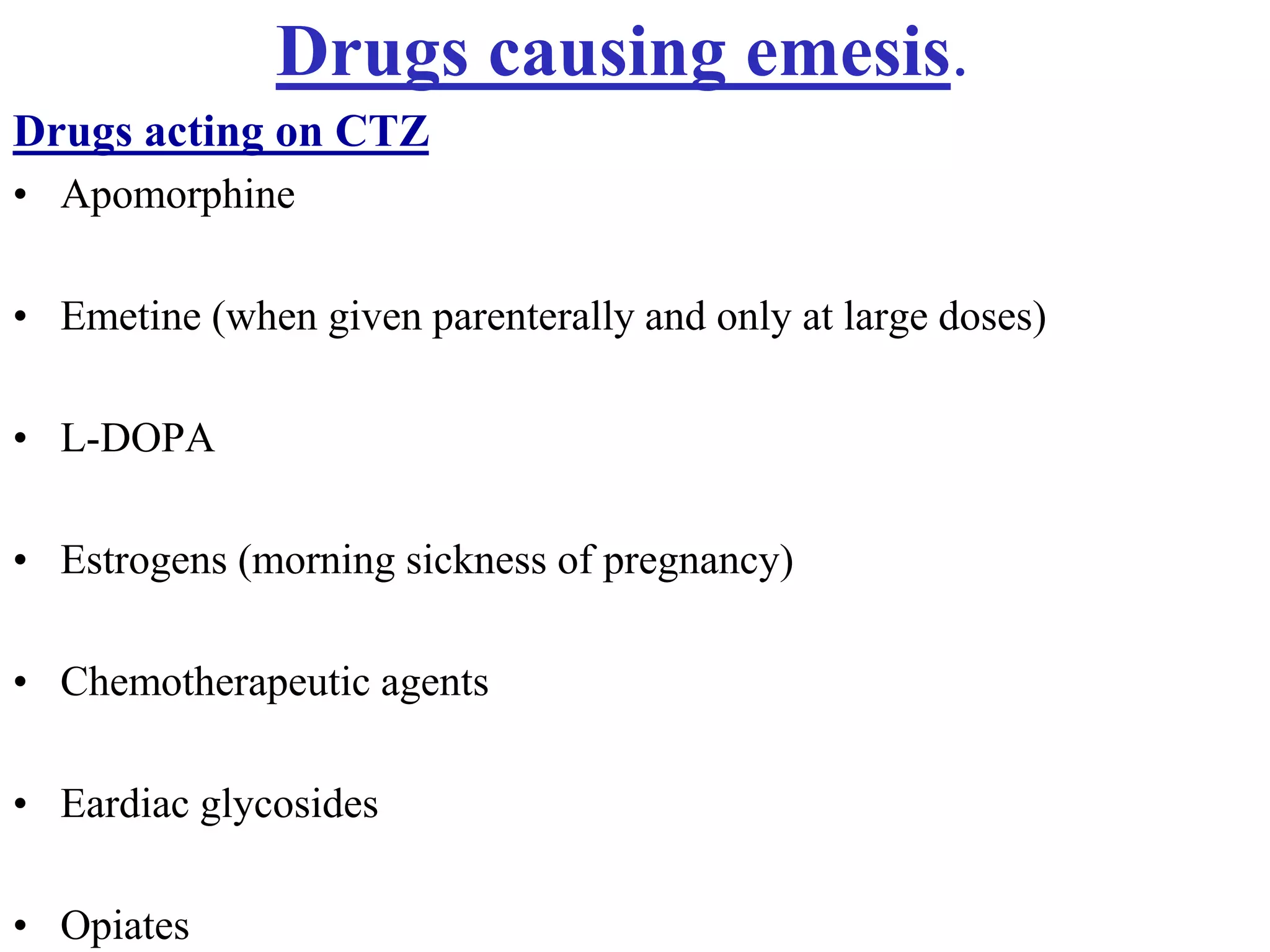
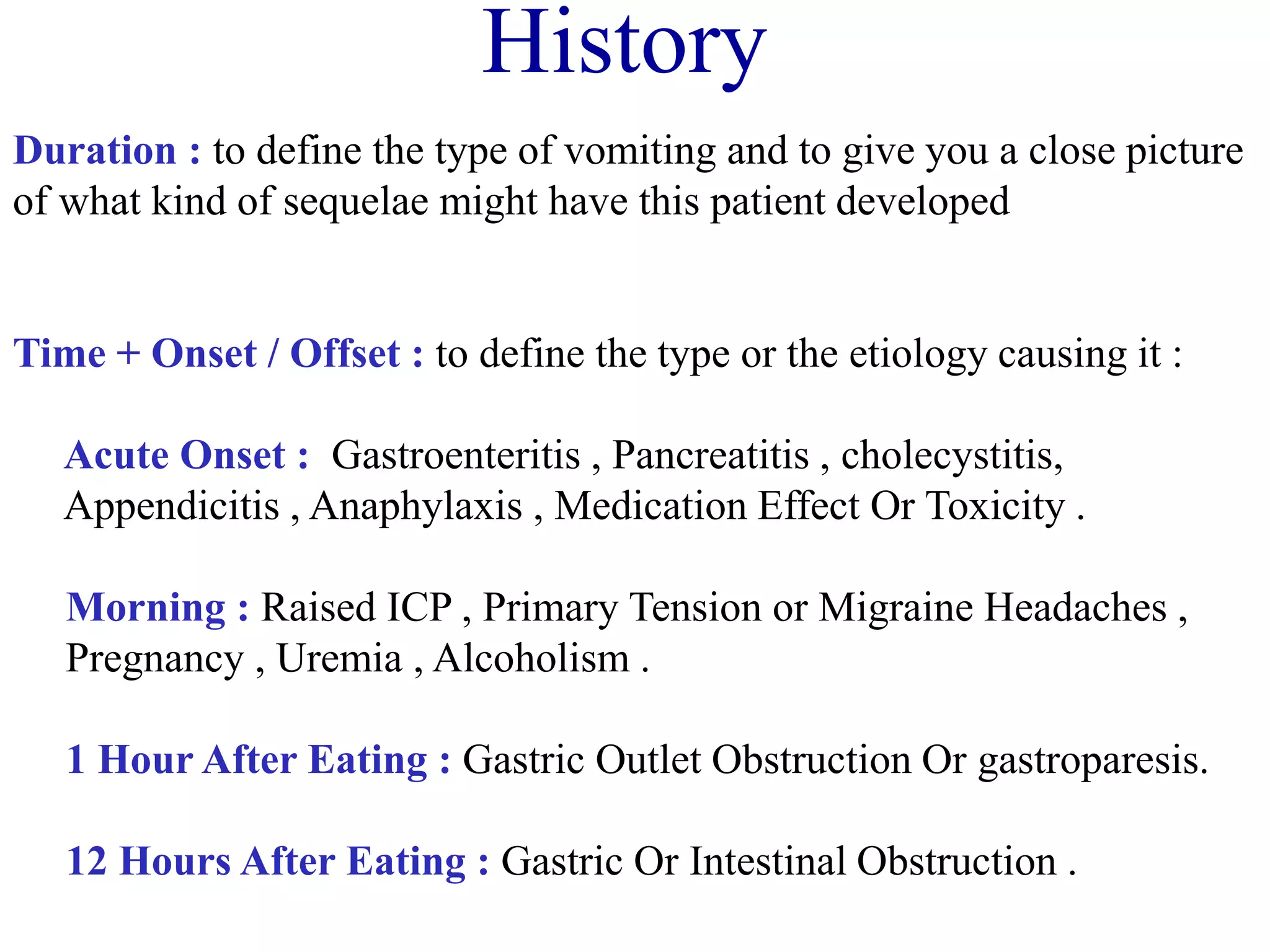
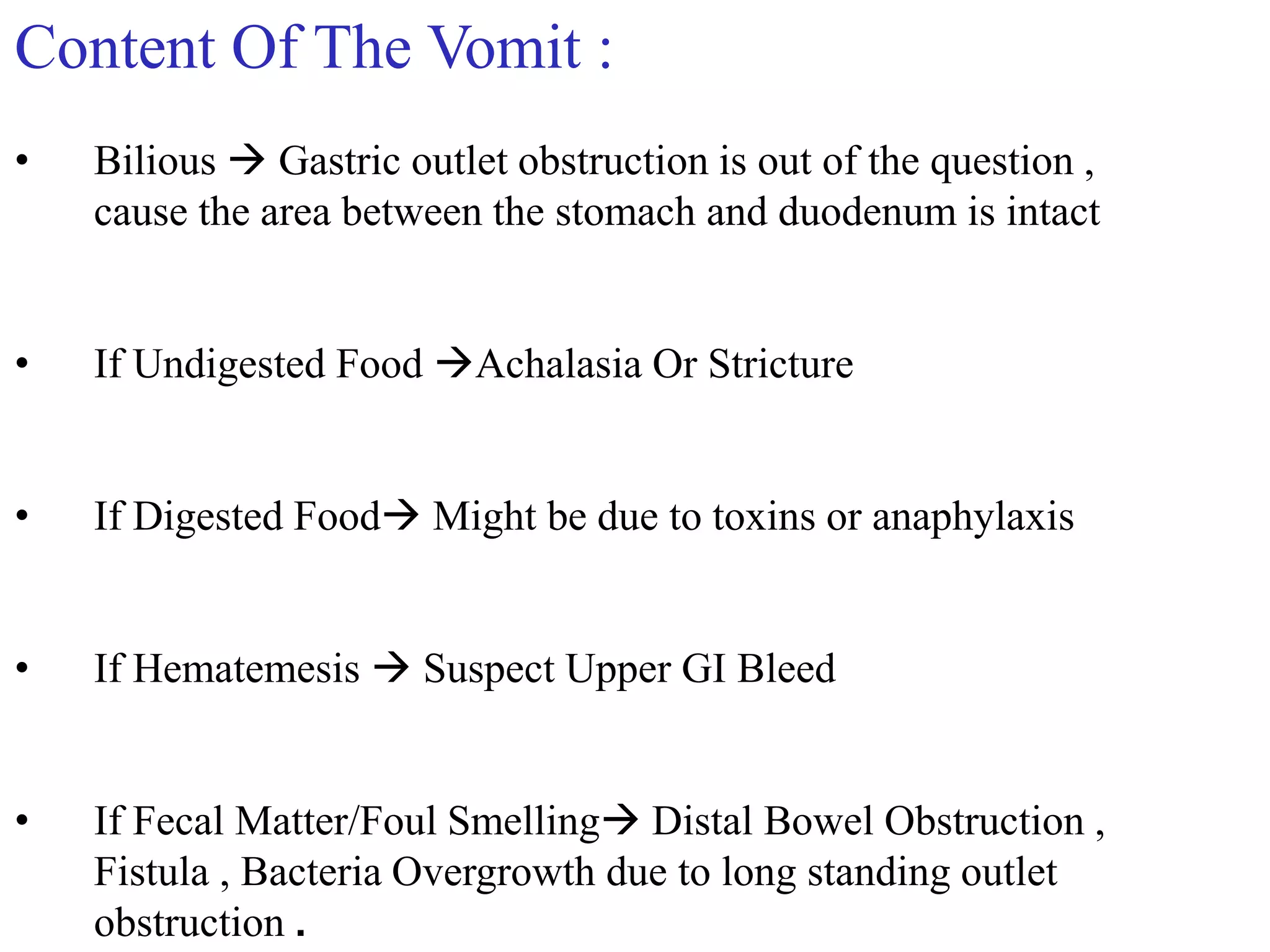
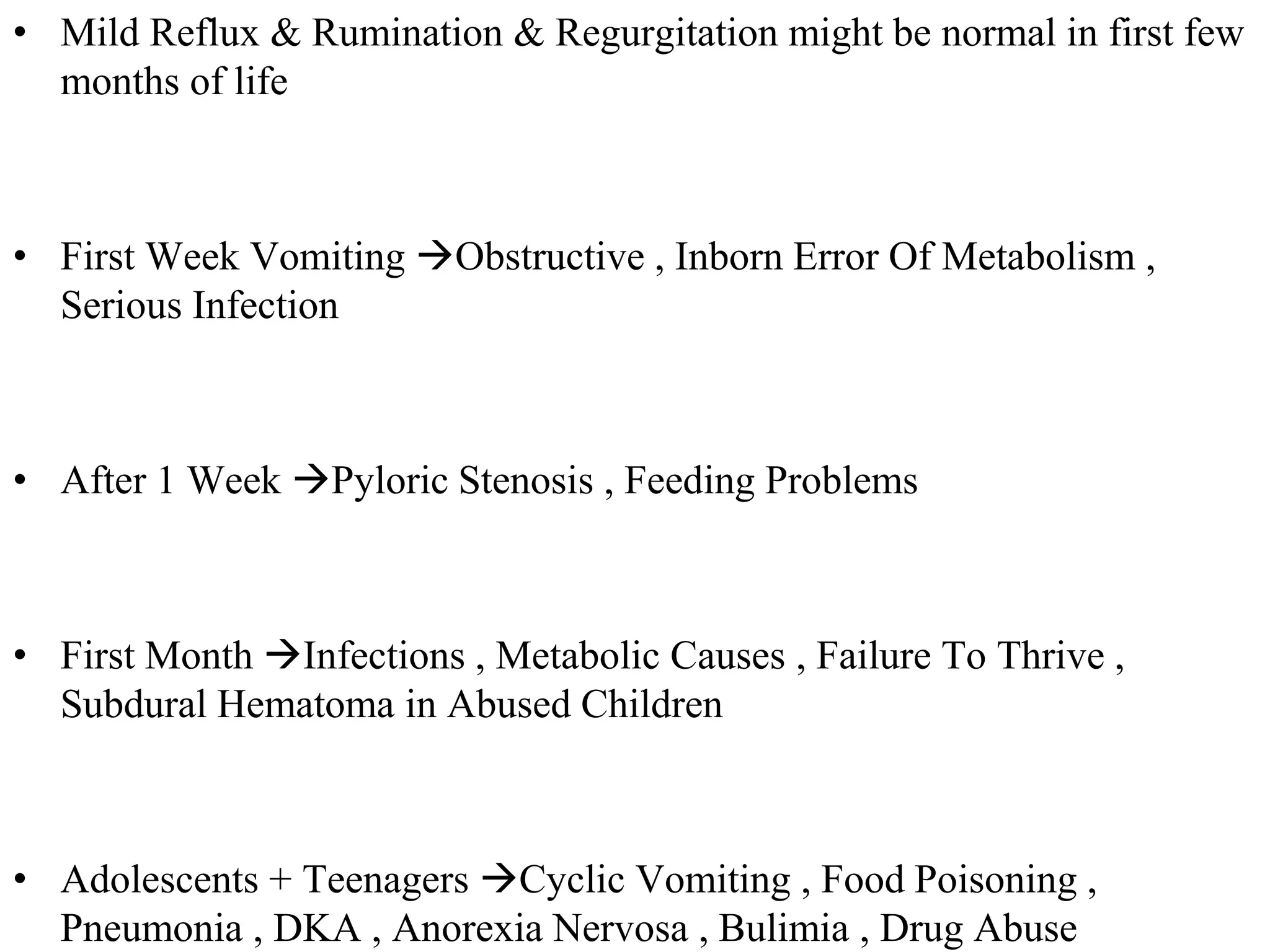
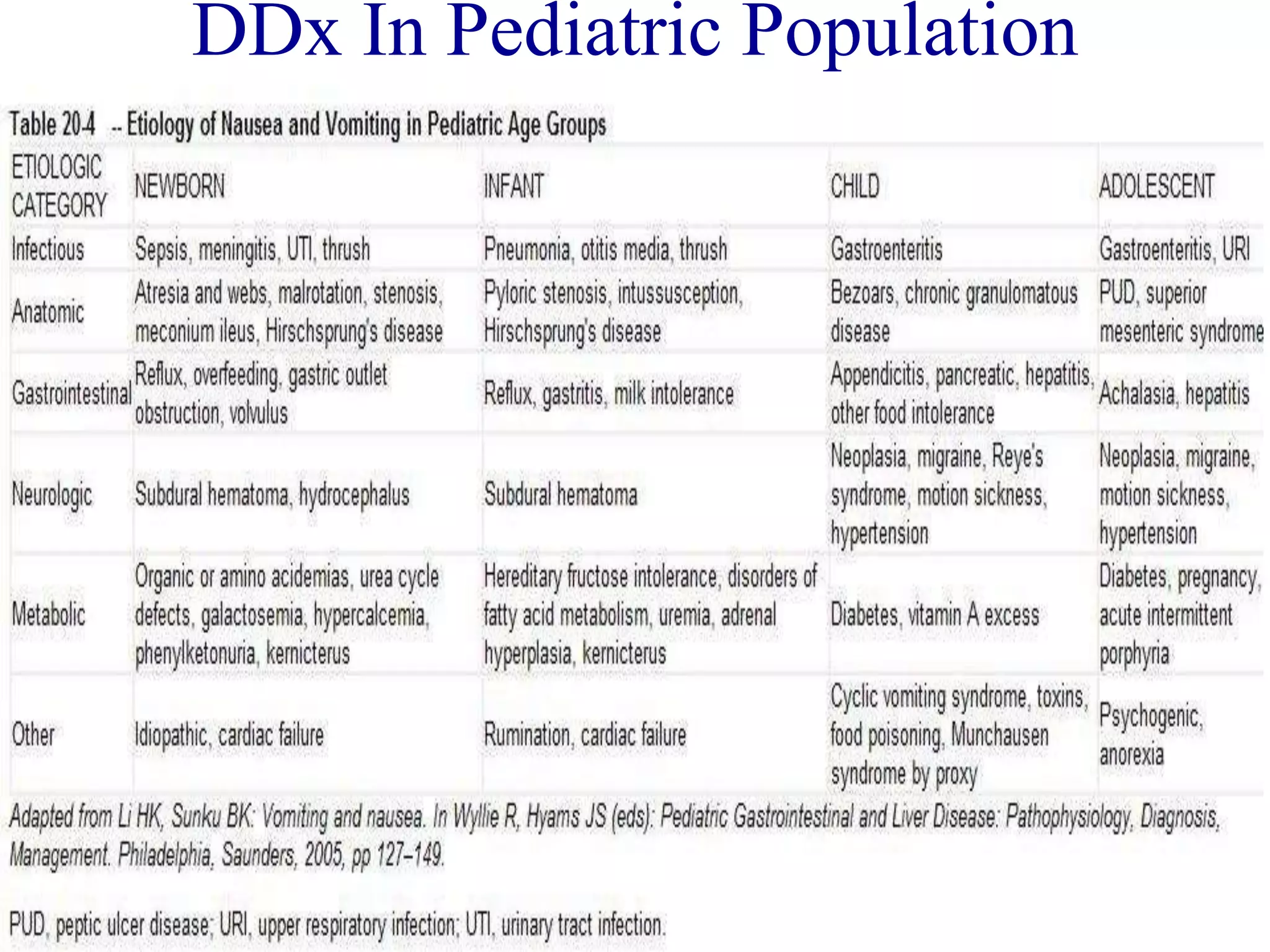
This document discusses nausea and vomiting. It begins by classifying vomiting as primary or secondary and acute or chronic. It then describes the reflex mechanism of vomiting which occurs in three phases: nausea, retching, and vomiting. Various causes of vomiting are provided for both general and pediatric populations. Evaluation involves taking a history and performing a physical exam and tests. The major types of antiemetics are described along with their mechanisms and clinical uses. Specific conditions like cyclic vomiting syndrome and nausea/vomiting of pregnancy are also discussed. The document concludes by outlining approaches to managing nausea and vomiting.