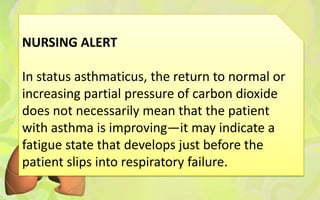
Status asthmaticus is a severe form of asthma that is unresponsive to usual drug therapy. It can be caused by infections, air pollutants, noncompliance with medications, or aspirin use in sensitive patients. Symptoms include rapid breathing, difficulty exhaling, anxiety, and fatigue. Management involves frequent monitoring, nebulized bronchodilators, corticosteroids, oxygen, suctioning secretions, and mechanical ventilation if needed. Nurses must closely watch for signs of respiratory failure.