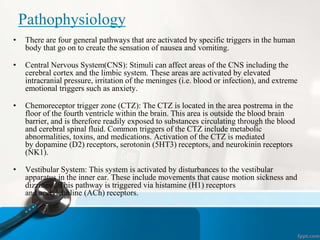
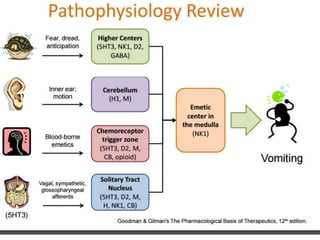
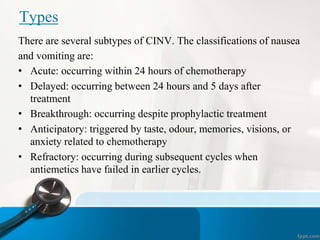
Nausea and vomiting are common symptoms that can be caused by many conditions. Nausea is an uneasiness of the stomach that often precedes vomiting, which is the forceful emptying of stomach contents through the mouth. Chemotherapy-induced nausea and vomiting (CINV) is a major side effect of cancer treatment. The risk of CINV depends on the specific chemotherapy drugs used and can be acute, delayed, or anticipatory. Effective prevention and treatment of CINV is important for maintaining quality of life. Medications that target different receptor pathways in the brain and gut are used as preventative and rescue therapies for CINV.