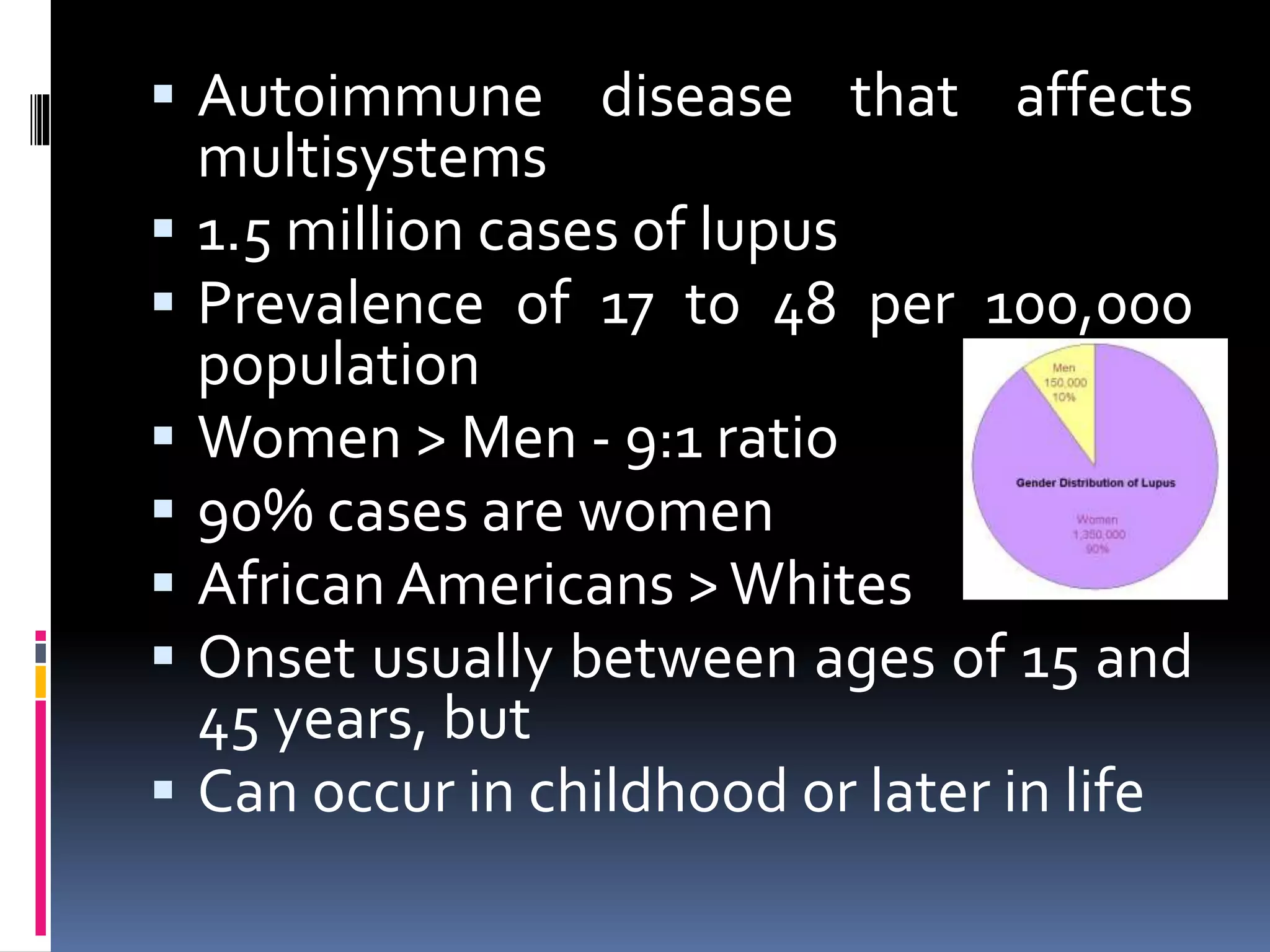
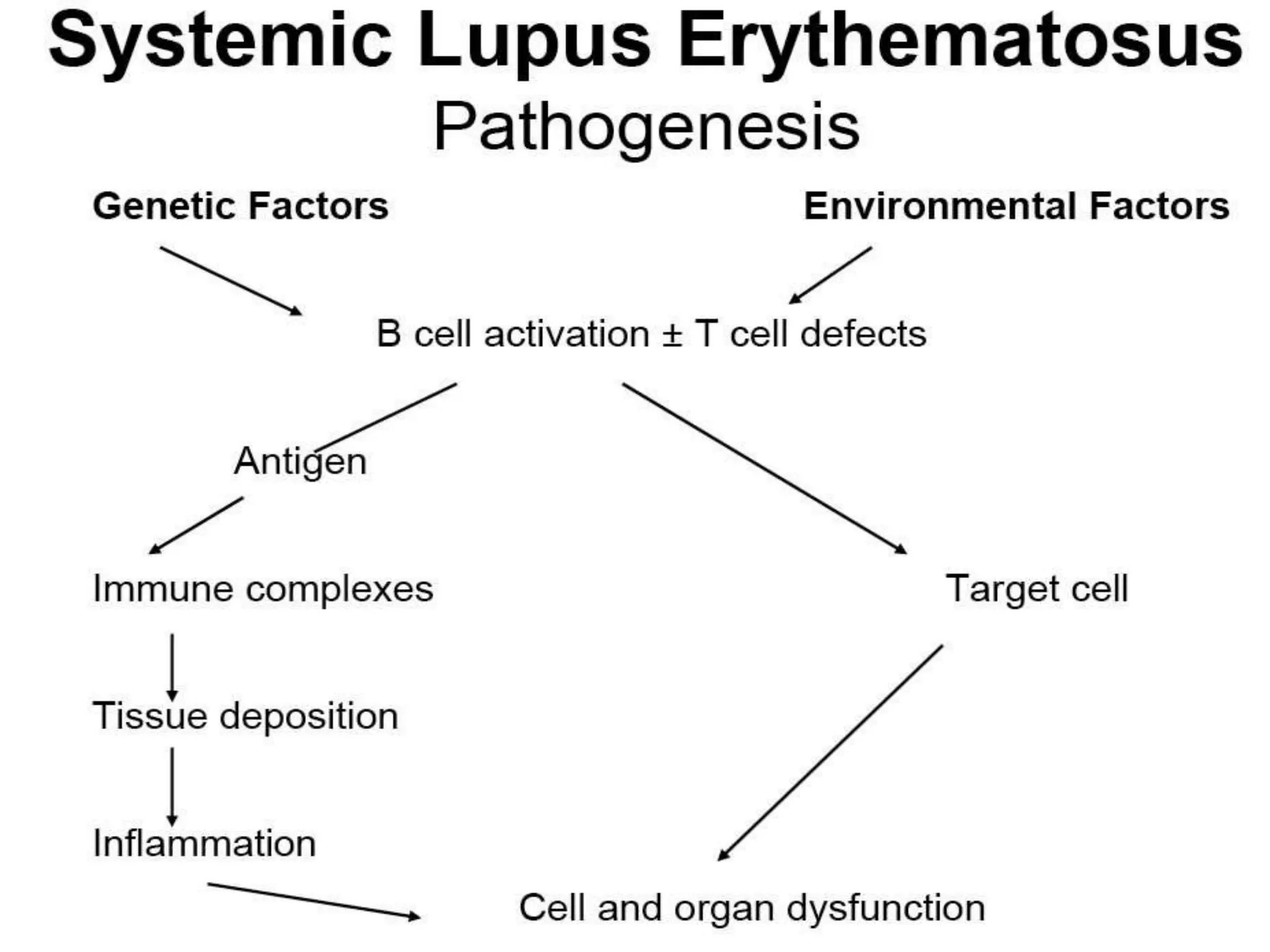
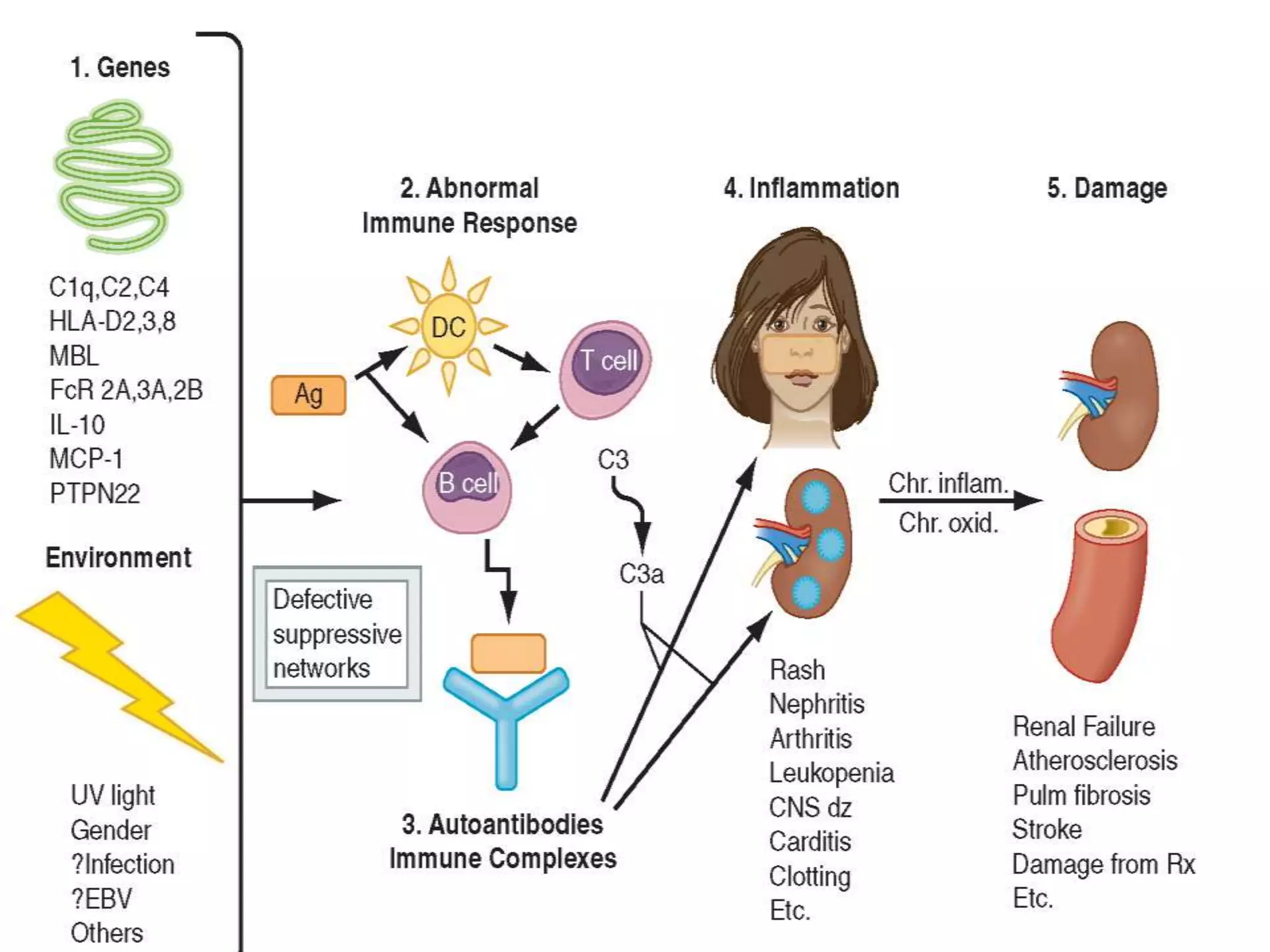
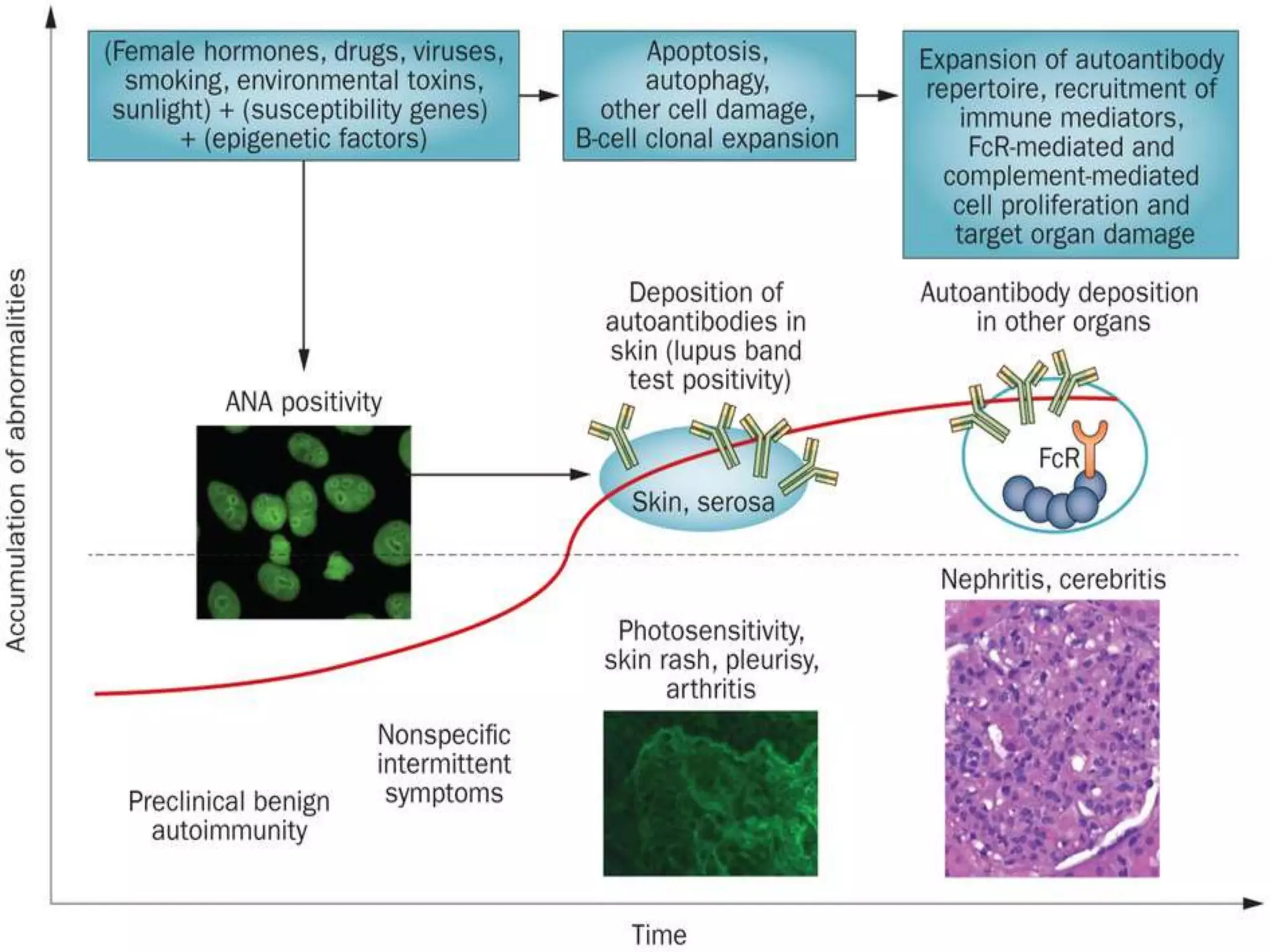
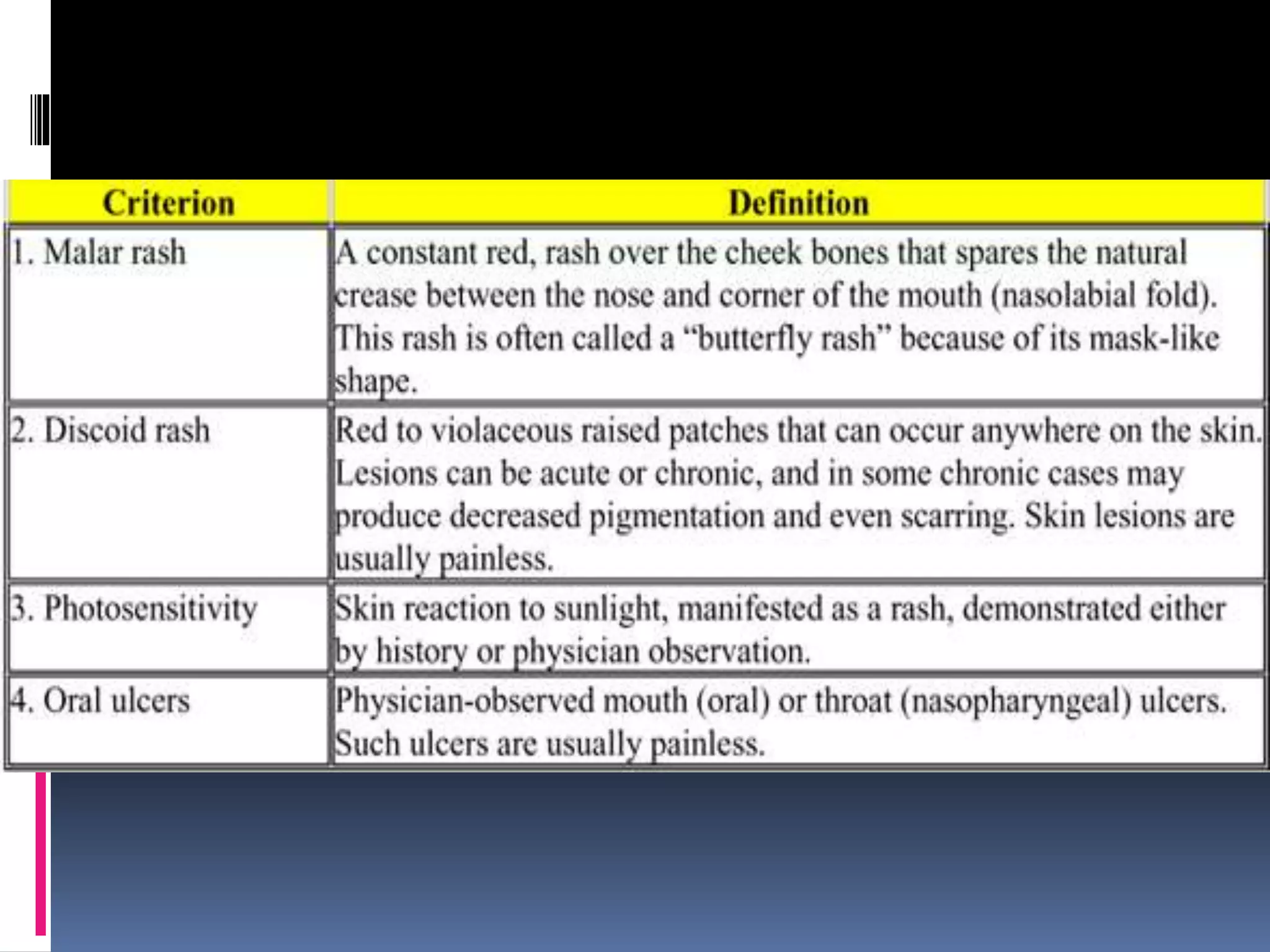
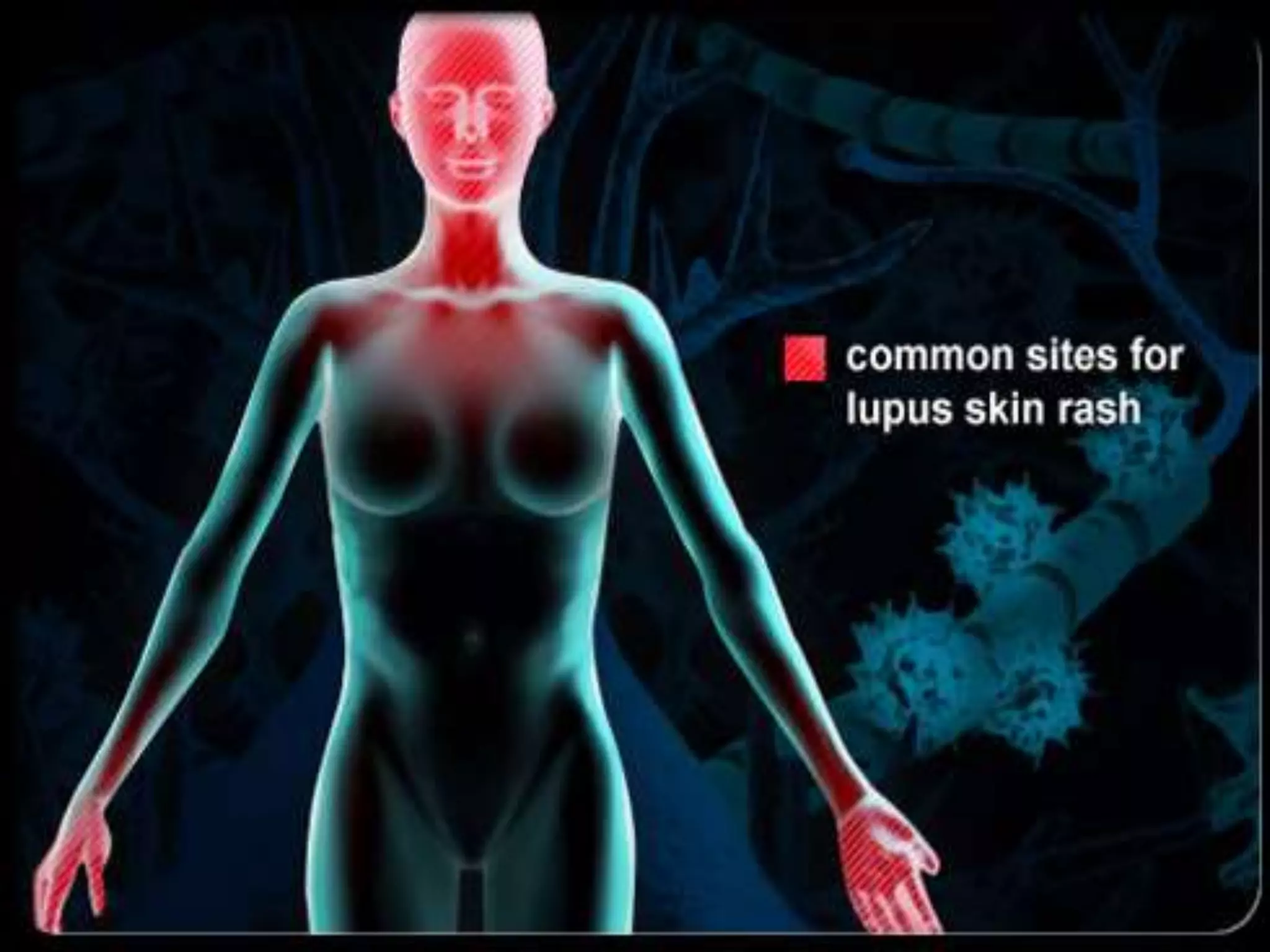
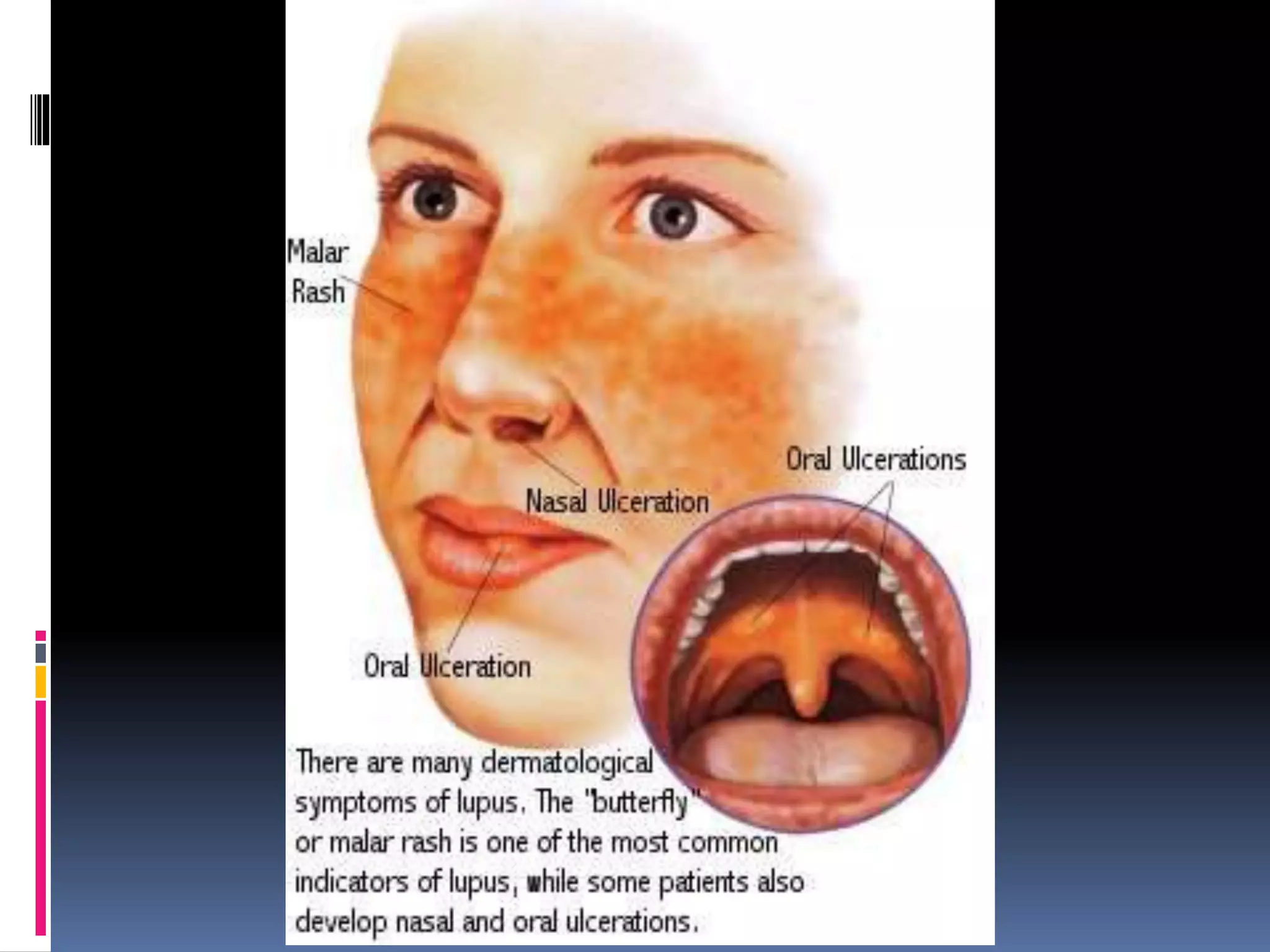
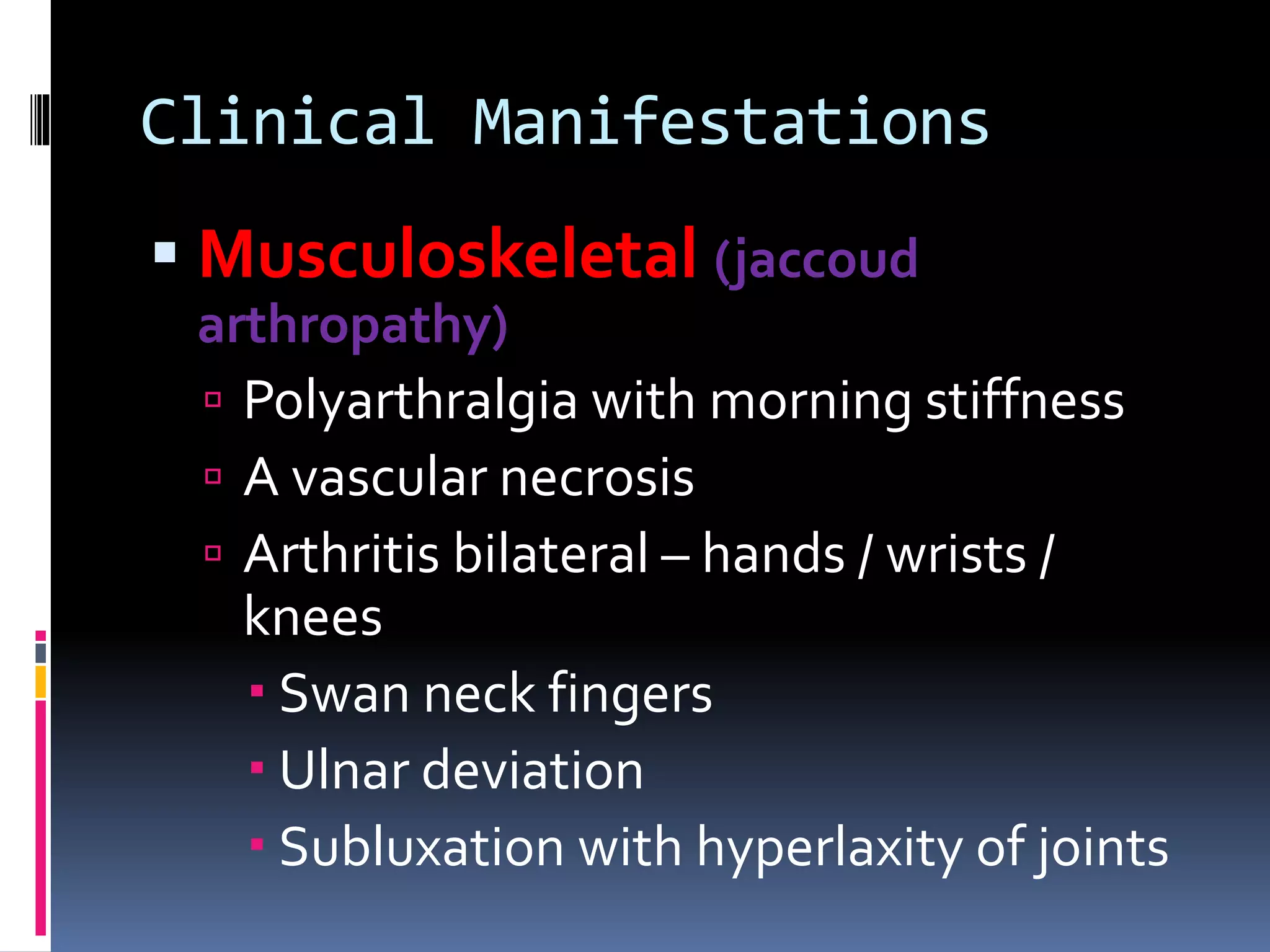
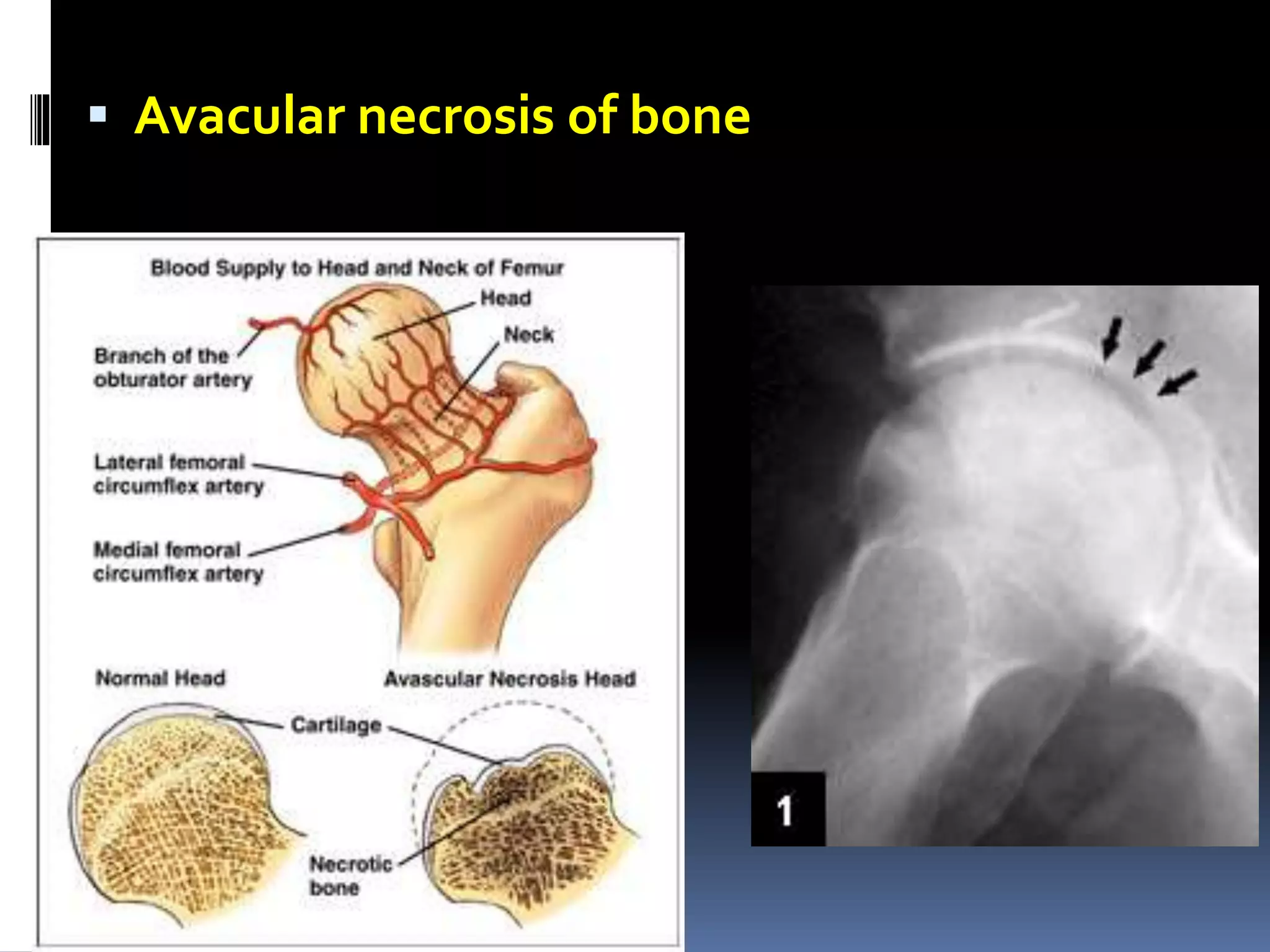
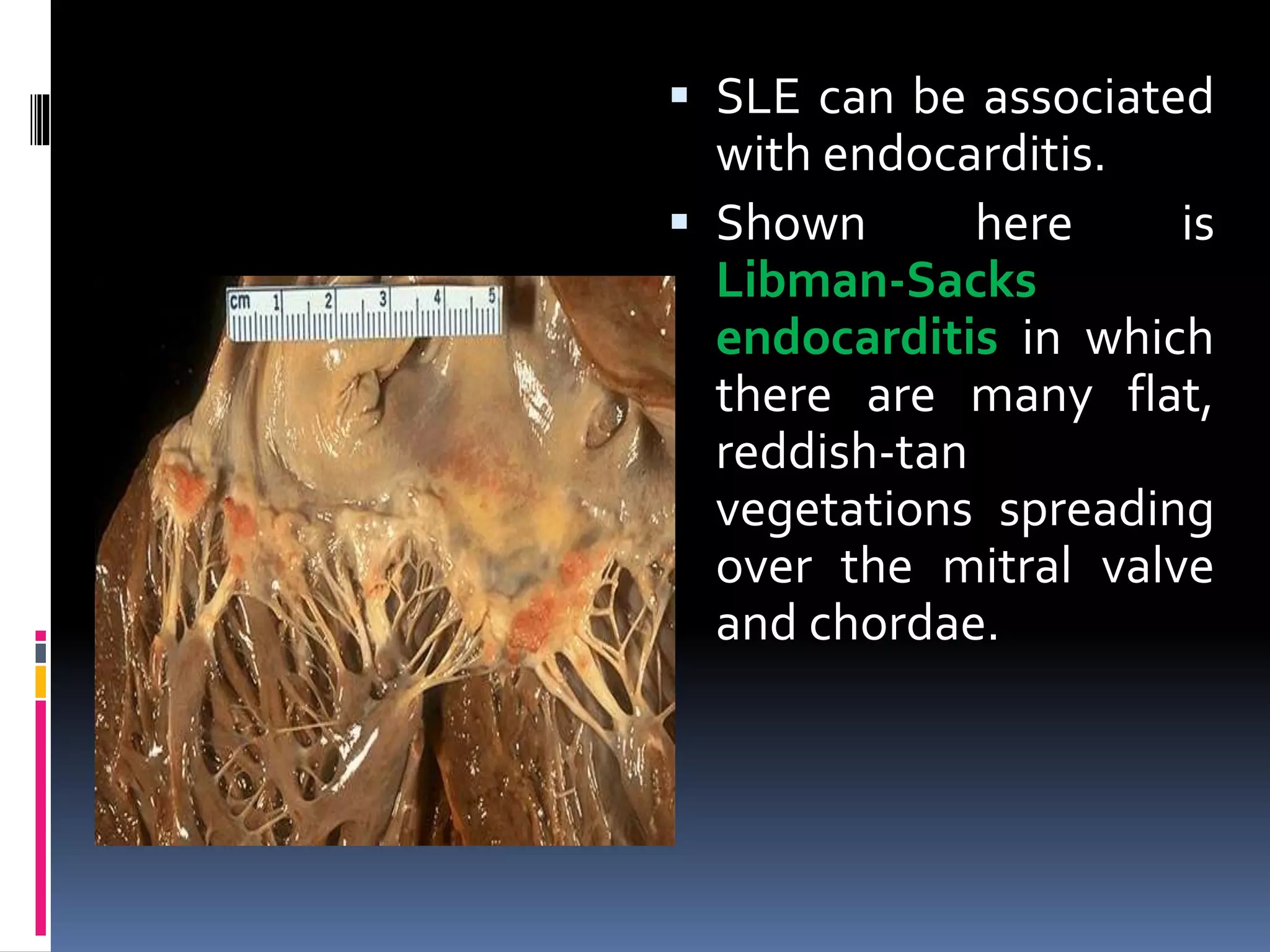
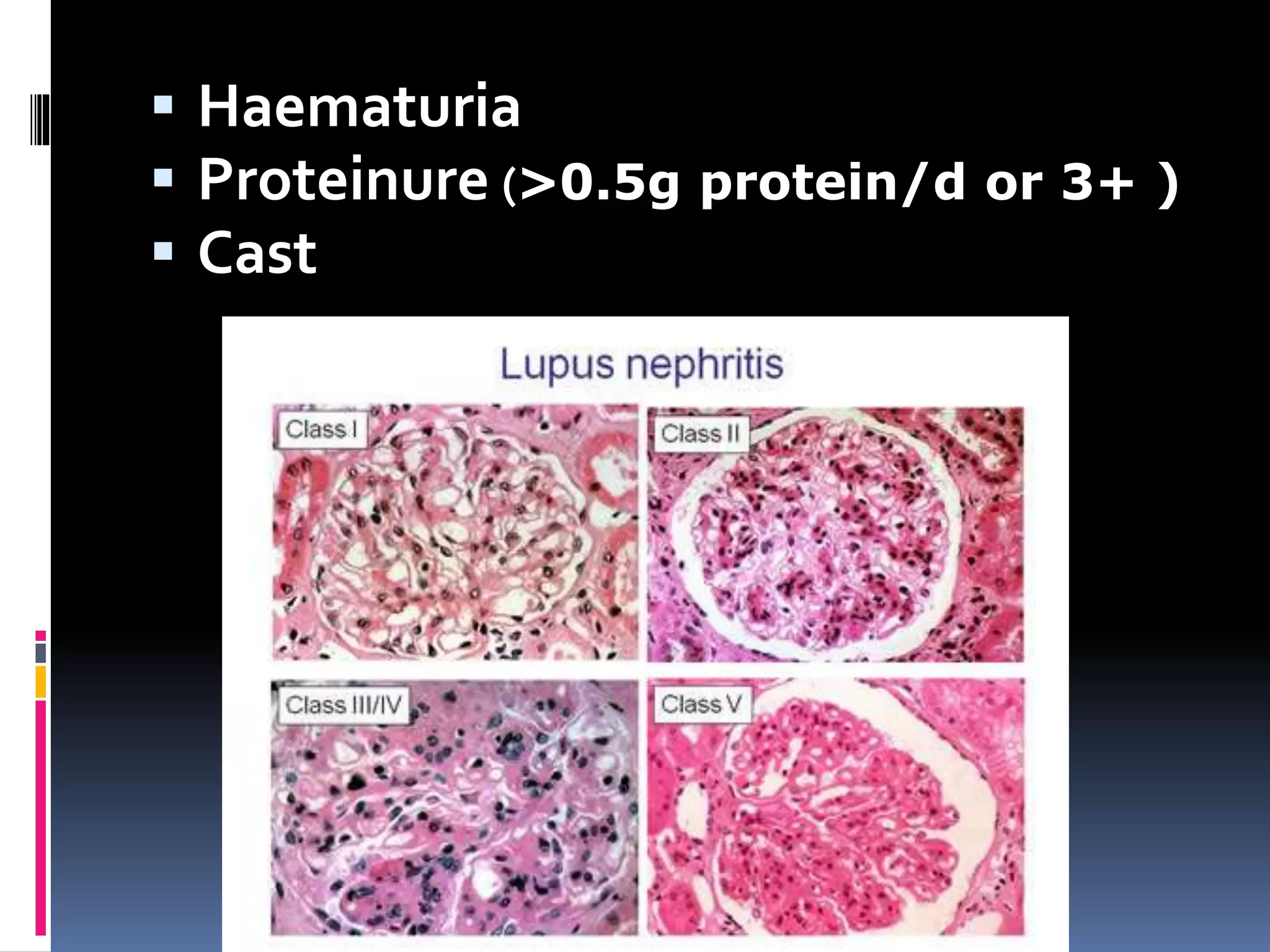
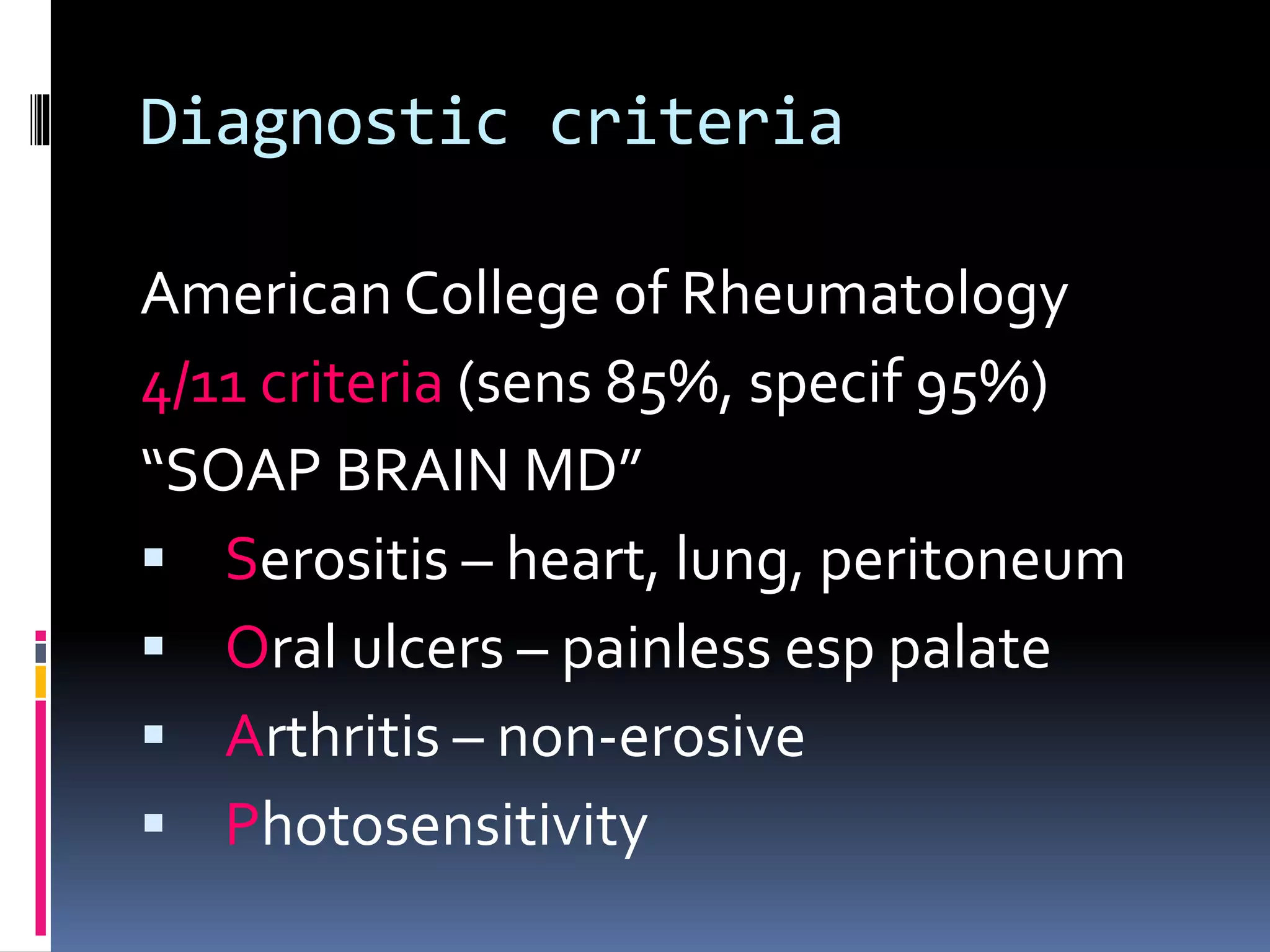
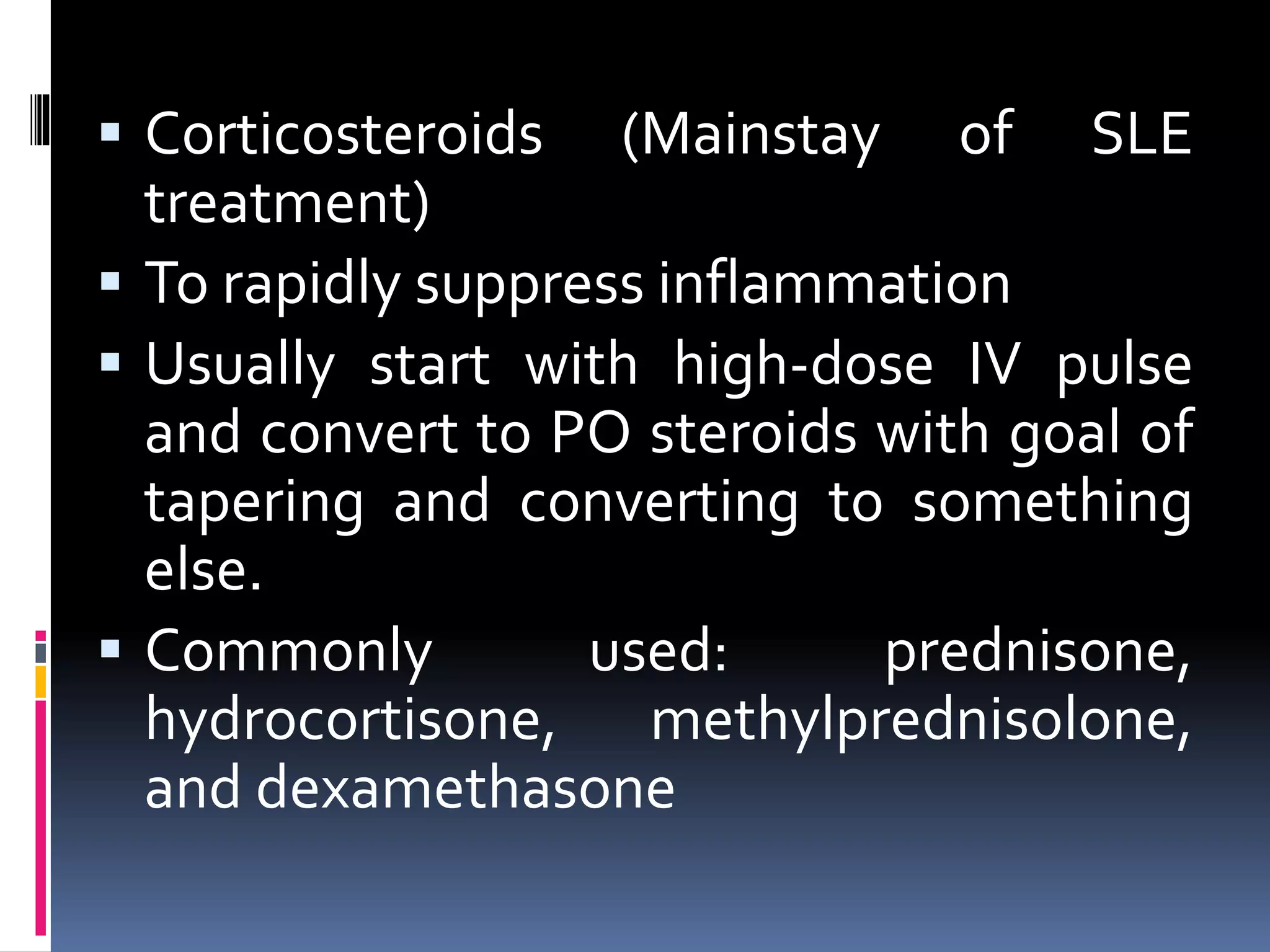
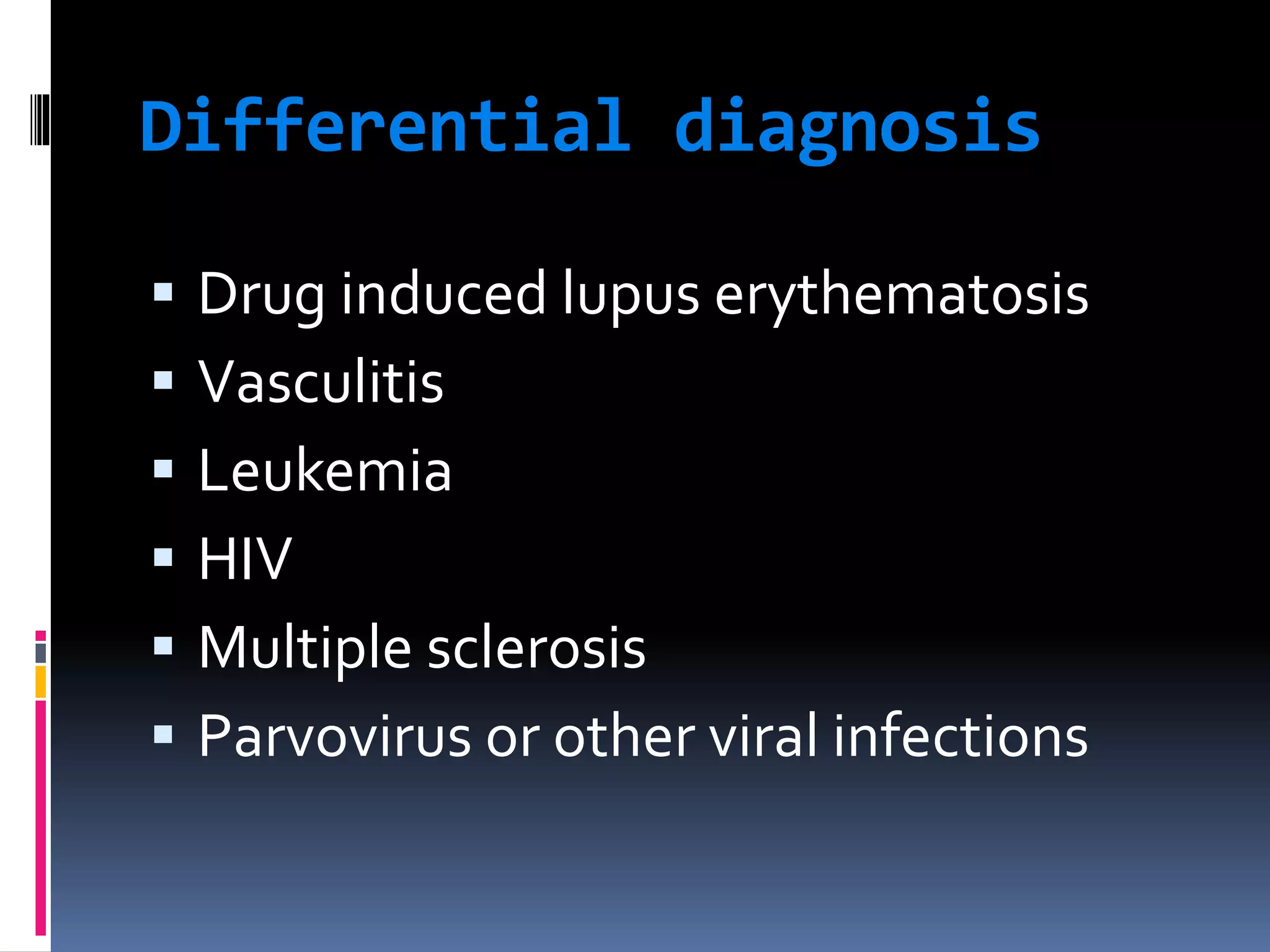
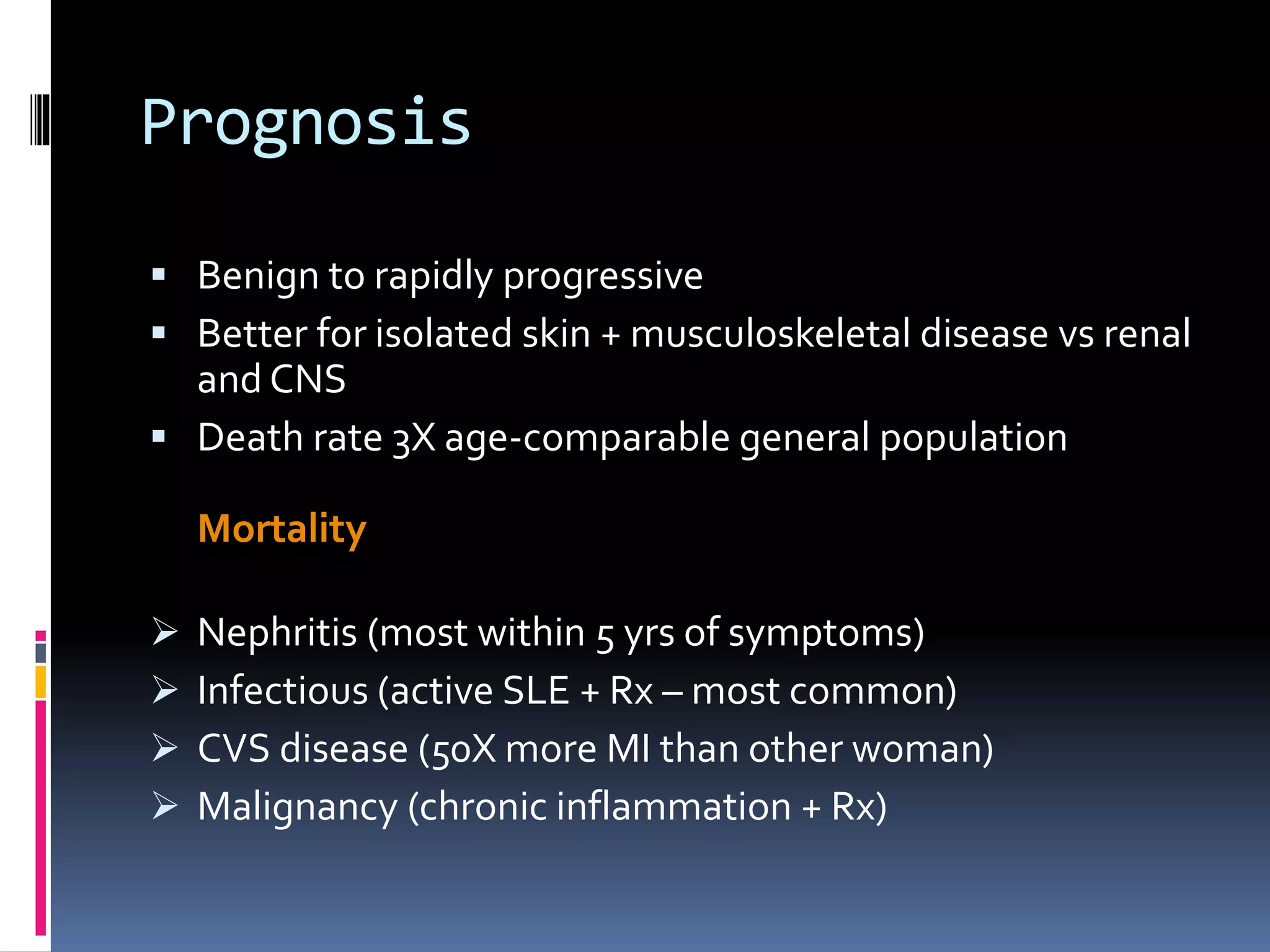
Systemic lupus erythematosus (SLE) is an autoimmune disease that can affect multiple organ systems. It is more prevalent in women and African Americans. Common initial symptoms include fatigue, fever, and weight loss. SLE can cause skin rashes, arthritis, serositis, renal disease, and neurological or hematological abnormalities. Treatment involves managing symptoms with NSAIDs, antimalarials, corticosteroids, and immunosuppressive drugs. Prognosis depends on organ involvement, with renal disease and CNS involvement carrying the worst outcomes.