This document provides an overview of vitiligo, including its definition, epidemiology, etiology, classification, clinical manifestations, pathogenesis, diagnosis, and treatment. Some key points are:
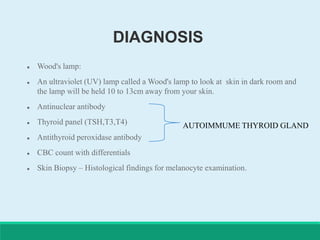
- Vitiligo is a skin condition characterized by loss of pigment-producing cells that results in white patches on the skin. It affects around 0.5-1% of the population worldwide.
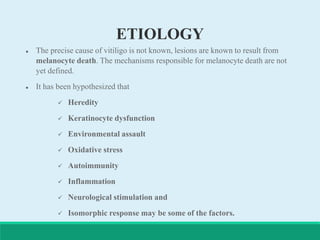
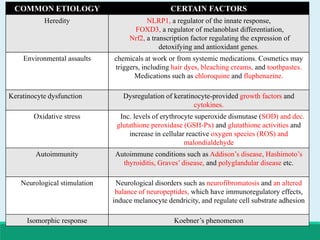
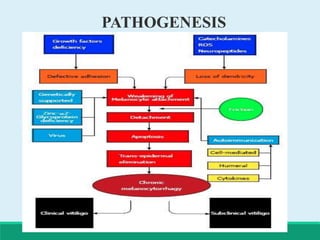
- The precise causes are unknown but are believed to involve genetic and environmental factors that may trigger an autoimmune response targeting melanocytes.
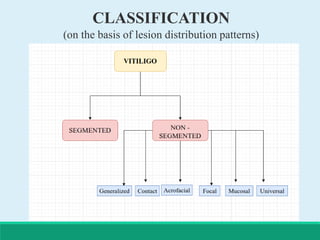
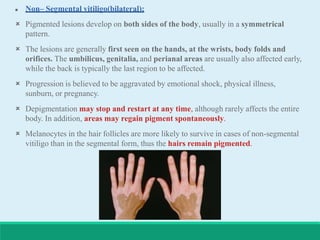
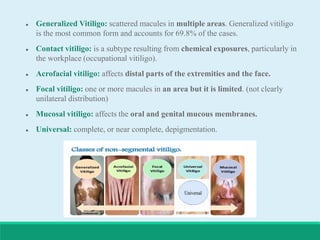
- Vitiligo can be classified based on the distribution of lesions as segmental, non-segmental, generalized, or other subtypes.
- Treatment options include phototherapy, topical