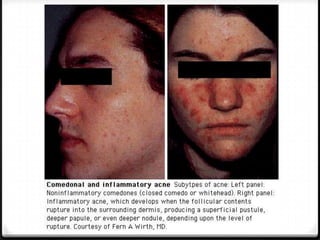
Acne vulgaris is a disorder of the pilosebaceous unit caused by increased sebum production, follicular hyperkeratinization, and bacterial colonization. It manifests as comedones, papules, pustules, nodules, and cysts. Treatment involves addressing underlying causes with topical retinoids, antibiotics, and oral antibiotics which reduce inflammation and P. acnes levels. For severe nodular cystic acne, oral isotretinoin is used which decreases sebum production and has anti-inflammatory effects.