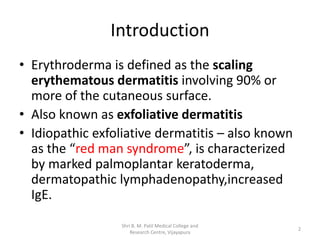
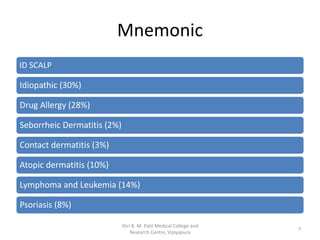
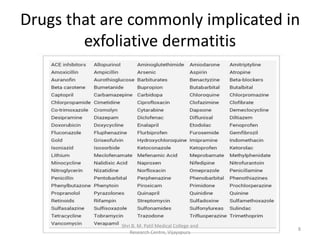
Erythroderma, also known as exfoliative dermatitis, involves extensive erythematous scaling affecting over 90% of the skin surface, often linked to various systemic conditions and characterized by high mortality rates. The document outlines pathophysiology, clinical features, differential diagnoses, investigations, and treatment options, emphasizing the importance of monitoring and addressing underlying causes. Key clinical symptoms include pruritis and generalized erythema, with treatment typically involving steroids, moisture maintenance, and addressing nutritional deficiencies.