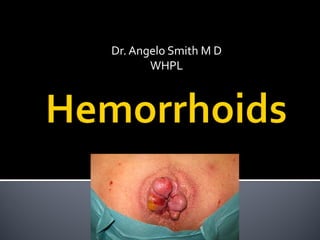
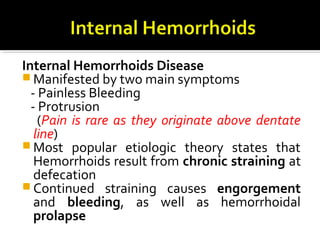
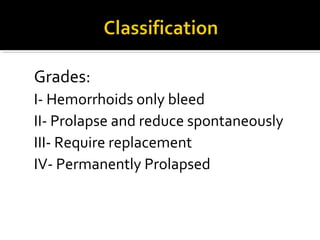
Hemorrhoids are enlarged or dilated veins in the lower rectum and anus. They commonly cause symptoms like painless rectal bleeding and protrusion from the anus. Risk factors include chronic straining during bowel movements, prolonged sitting, obesity, and pregnancy. Treatment ranges from lifestyle and dietary modifications to minimally invasive procedures or surgery. Surgical hemorrhoidectomy is reserved for grades III-IV hemorrhoids.