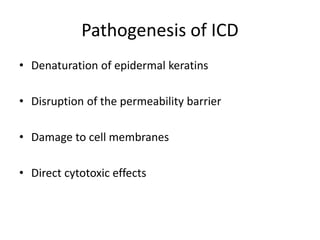
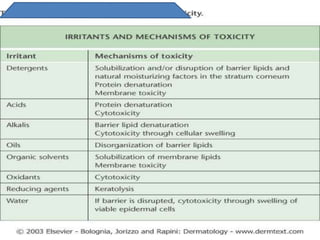
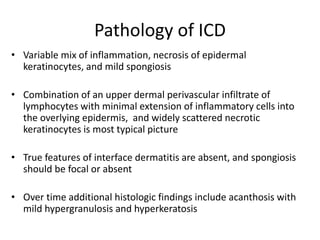
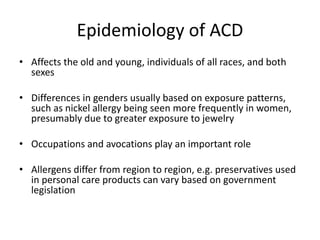
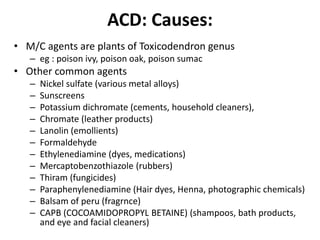
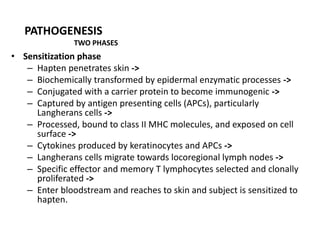
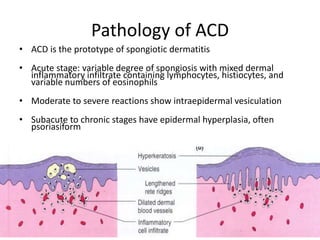
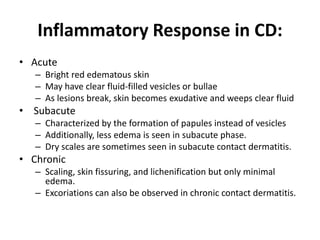
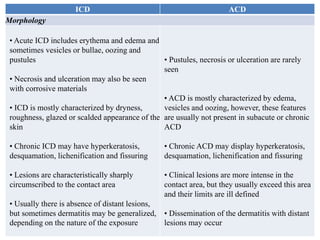
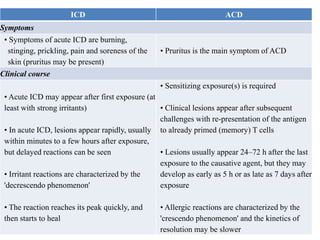
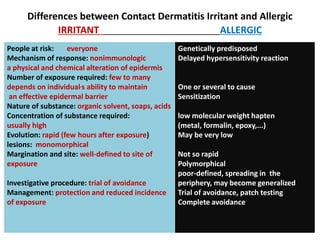
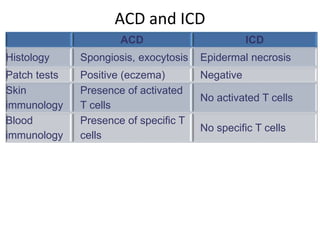
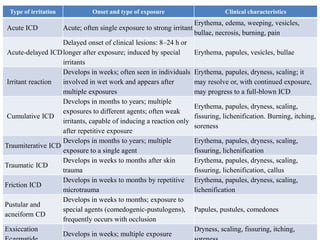
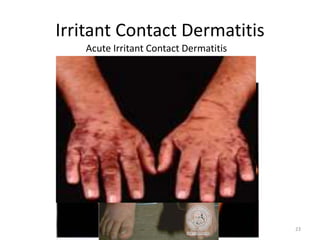
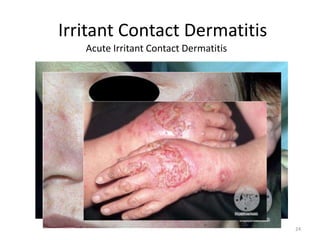
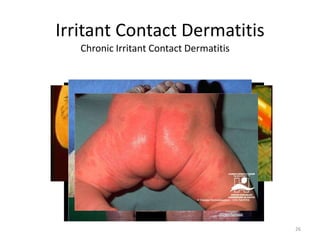
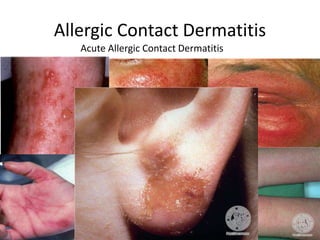
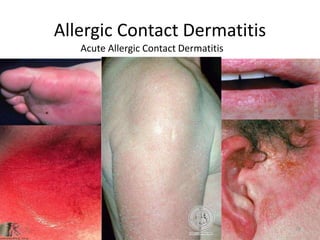
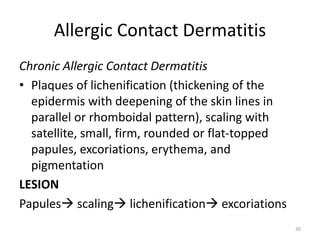
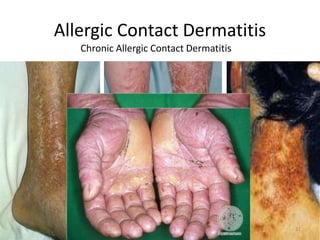
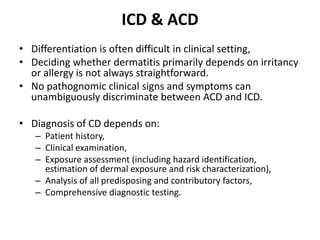
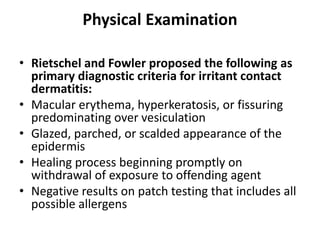
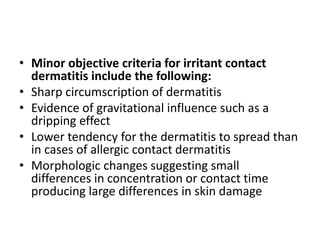
This document discusses irritant contact dermatitis (ICD) and its causes, pathogenesis, epidemiology, clinical manifestations, and differences from allergic contact dermatitis. ICD is caused by contact with irritating chemicals, physical agents, or microbes in the environment. It results in skin lesions, mucosa lesions, or semi-mucosa lesions through irritant pathogenic mechanisms. ICD presents with erythema, edema, weeping lesions, vesicles or bullae and the reaction peaks quickly then starts to heal. In contrast, allergic contact dermatitis involves a sensitization phase and elicitation phase and presents with pruritus, vesicles and oozing lesions that spread beyond the contact area.