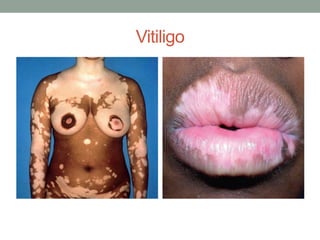
Vitiligo is a condition characterized by loss of skin pigmentation. It results from the absence of melanocytes in the epidermis. There are several types classified by the extent and location of depigmentation. The cause is thought to be autoimmune, neural, or related to toxic melanin precursors. Treatment aims to restore pigmentation and is initially topical steroids, phototherapy, or laser treatments. For more extensive vitiligo, depigmentation of the entire skin or systemic corticosteroids may be used.