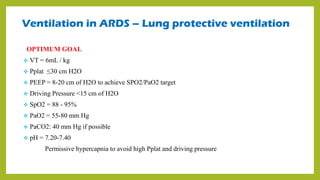
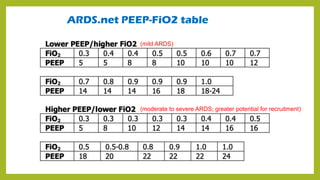
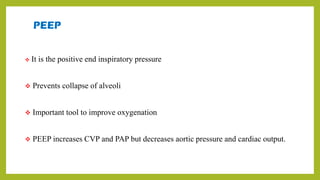
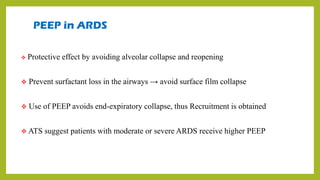
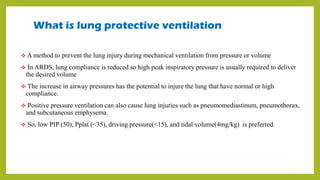
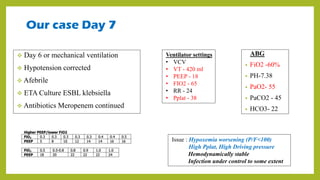
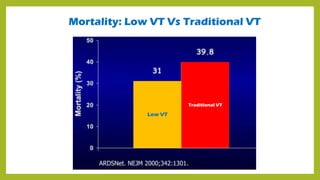
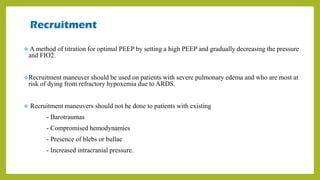
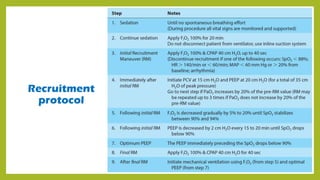
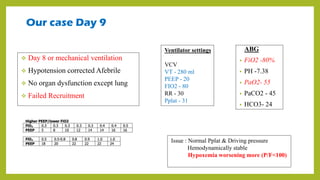
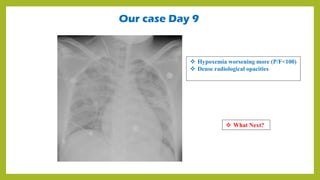
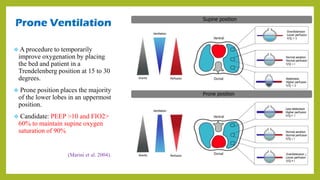
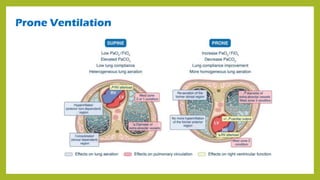
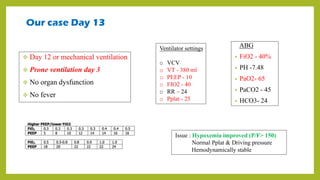
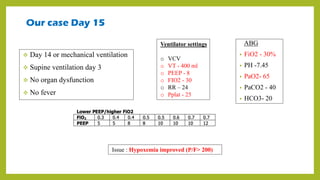
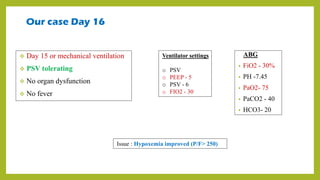
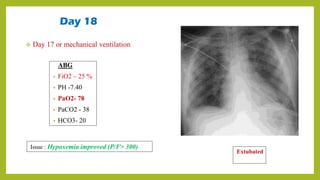
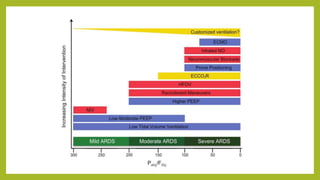
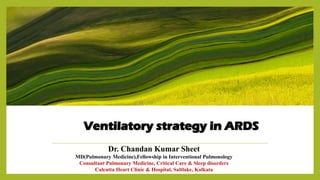
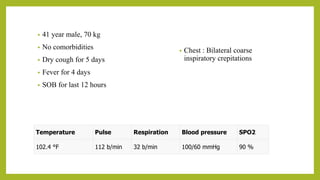
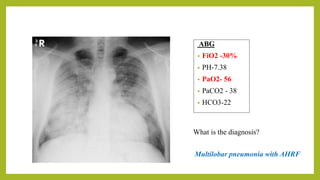
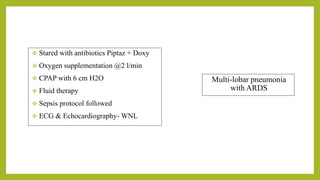
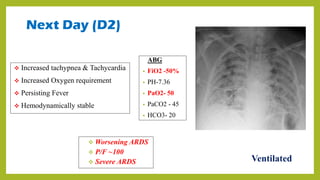
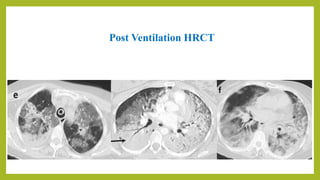
The document outlines a comprehensive approach to managing Acute Respiratory Distress Syndrome (ARDS), detailing definitions, pathophysiology, and ventilatory strategies with specific case examples. It emphasizes lung protective ventilation techniques, recruitment maneuvers, and the significance of optimal PEEP settings to improve patient outcomes. The progression of a specific patient's case illustrates various treatment adjustments and their impact on oxygenation and ventilation parameters over time.

![Ventilation in ARDS – Lung Protective Ventilation
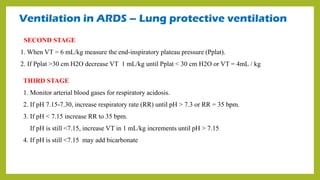
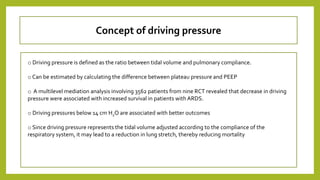
FIRST STAGE
1. Calculate Predicted body weight
Male : PBW = 50 + [2.3 x (Height in inch – 60)]
Female : PBW = 45.5 + [2.3 x (Height in inch – 60)]
2. Mode : VCV
3. Set initial tidal volume (VT) at 8 mL/kg PBW.
4. PEEP at 5 cm H2O ( Recent Guidelines 8-20cm of H2O)
5. Lowest FiO2 that achieves an SpO2 of 88-95%.
6. RR : 20-35/min
7. Inspiratory time: 0.5-0.8 s
8. Reduce VT by 1 mL/kg every 2 hrs. until VT = 6 mL/kg.](https://image.slidesharecdn.com/ardsventilationchandan-240627174315-716e403a/85/VENTILATORY-STRATEGY-IN-ARDS-CHANDAN-pdf-14-320.jpg)