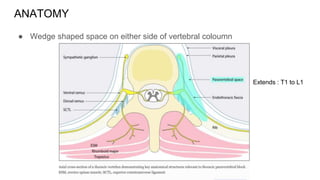
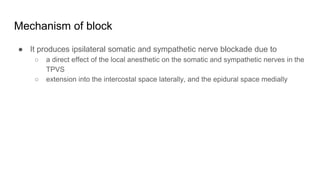
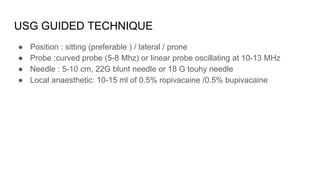
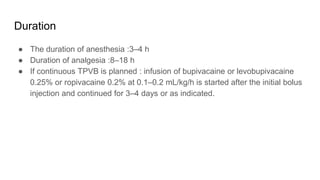
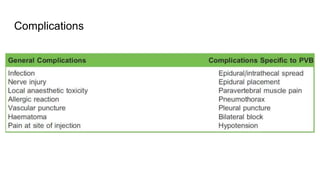
USG-guided thoracic paravertebral block is a technique for injecting local anesthetic alongside the thoracic vertebrae to provide unilateral somatic and sympathetic nerve blockade. It involves visualizing the transverse processes and pleura with ultrasound and inserting a needle in plane to deposit local anesthetic in the paravertebral space. When performed correctly, it provides effective postoperative analgesia for thoracic and upper abdominal surgeries for 3-4 hours with a single injection or up to 3-4 days with a catheter. Complications are rare if real-time ultrasound guidance is used.