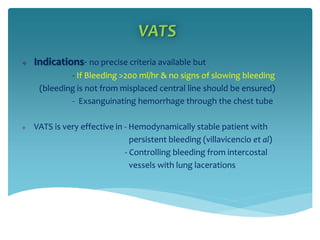
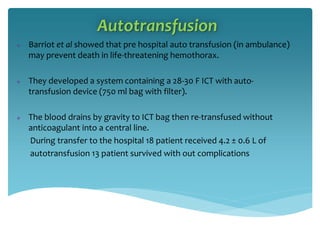
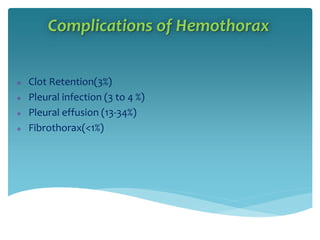
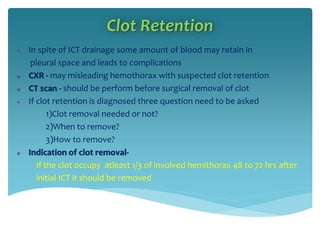
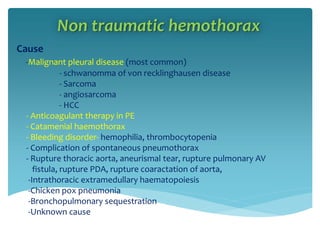
This document discusses various types and causes of hemothorax. It defines hemothorax as blood in the pleural space and lists trauma, medical conditions, and iatrogenic causes. Treatment options discussed include tube thoracostomy for drainage, VATS for bleeding control, and CT-guided arterial embolization. Complications like clot retention, empyema, and fibrothorax are described. Nontraumatic causes such as malignancy, anticoagulation therapy, and endometriosis are also summarized.








![Nontraumatic hemothorax..cont..
Diagnosis- Pleural fluid Haematocrit - > 50% of blood
Or
Pleural fluid RBC > 50% of blood
o [a rough estimation of haematocrit can be obtained by pleural fluid
RBC/1,OO,OOO ]
o [ hematocrit <5 % in pleural fluid may look like blood]
Treatment
- ICT
- thoracotomy / VATS- [If bleeding >100ml/ hr]
- Angiographic embolization [if bleeding from intercostal artery]](https://image.slidesharecdn.com/hemothorax-190330200130/85/Hemothorax-17-320.jpg)

![Catamenial Hemothorax
Unusual
Occurs in conjunction with menstruation
Associated with endometriosis
Rt hemithorax almost always involved
Diaphragmatic fenestration and pleuro-peritonial communication
demonstrated in some patient
Most patient have pleural endometriosis
Treatment
- Suppression of ovulation by-OCP, progesterone
- Suppression of gonadotrophin by –danazole, GnRH
- Pleurodesis [if hormonal therapy fails]
- THBSO](https://image.slidesharecdn.com/hemothorax-190330200130/85/Hemothorax-19-320.jpg)

