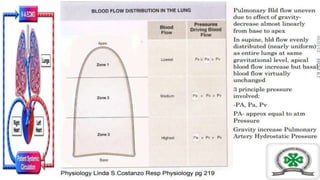
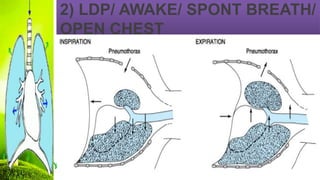
This document discusses one lung ventilation (OLV), which involves ventilating one lung while collapsing the other lung to provide surgical access. It begins by outlining the principles and history of OLV. It then discusses the advantages and absolute/relative indications for OLV. The document goes on to explain the changes in respiratory physiology and ventilation-perfusion matching that occur with OLV compared to two lung ventilation in various positions (awake, anesthetized, open chest). It also covers hypoxic pulmonary vasoconstriction and strategies to optimize oxygenation during OLV.