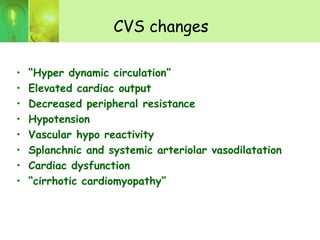
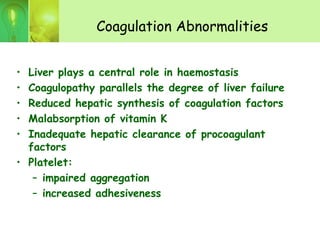
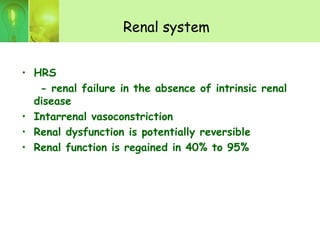
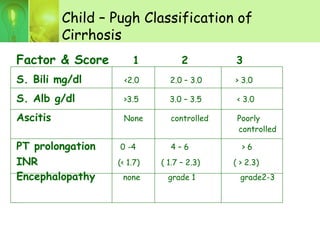
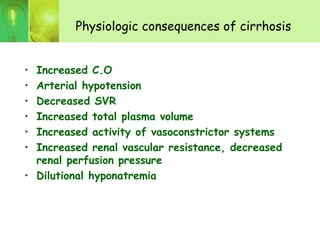
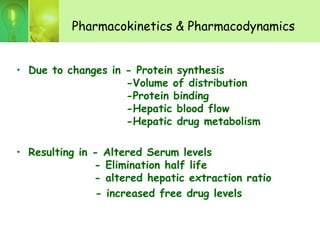
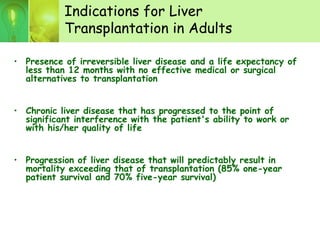
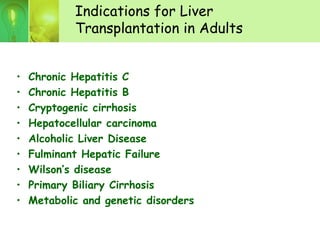
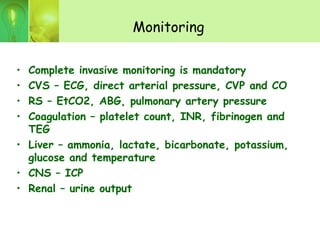
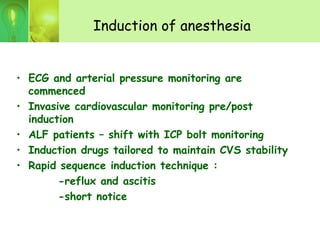
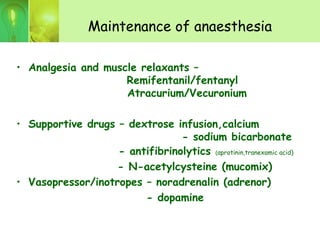
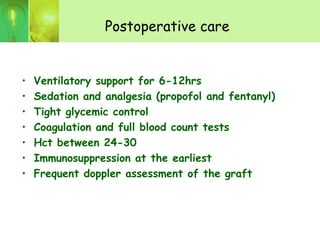
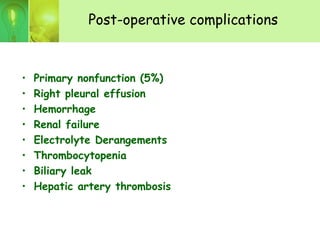
Liver transplantation involves complex anesthesia management due to physiological changes from cirrhosis and transplantation. Key aspects include invasive hemodynamic monitoring, management of coagulopathy and fluid shifts, and intensive care of recipients post-operatively due to risks of primary nonfunction, bleeding, infection and renal failure. Outcomes have improved dramatically with advances like cyclosporine in 1979 and living donor transplantation, with 1-year survival rates now over 90% for liver transplantation.