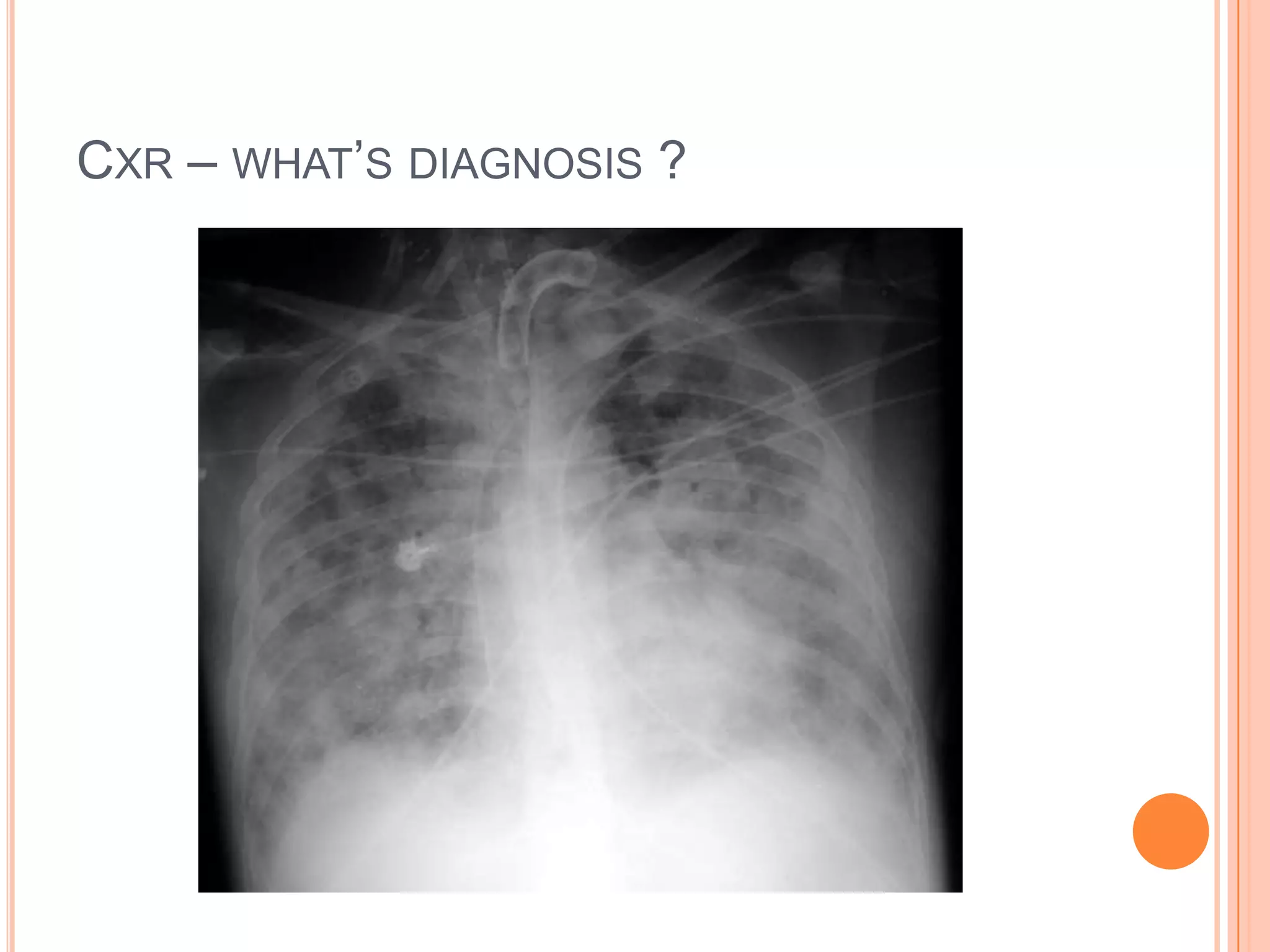
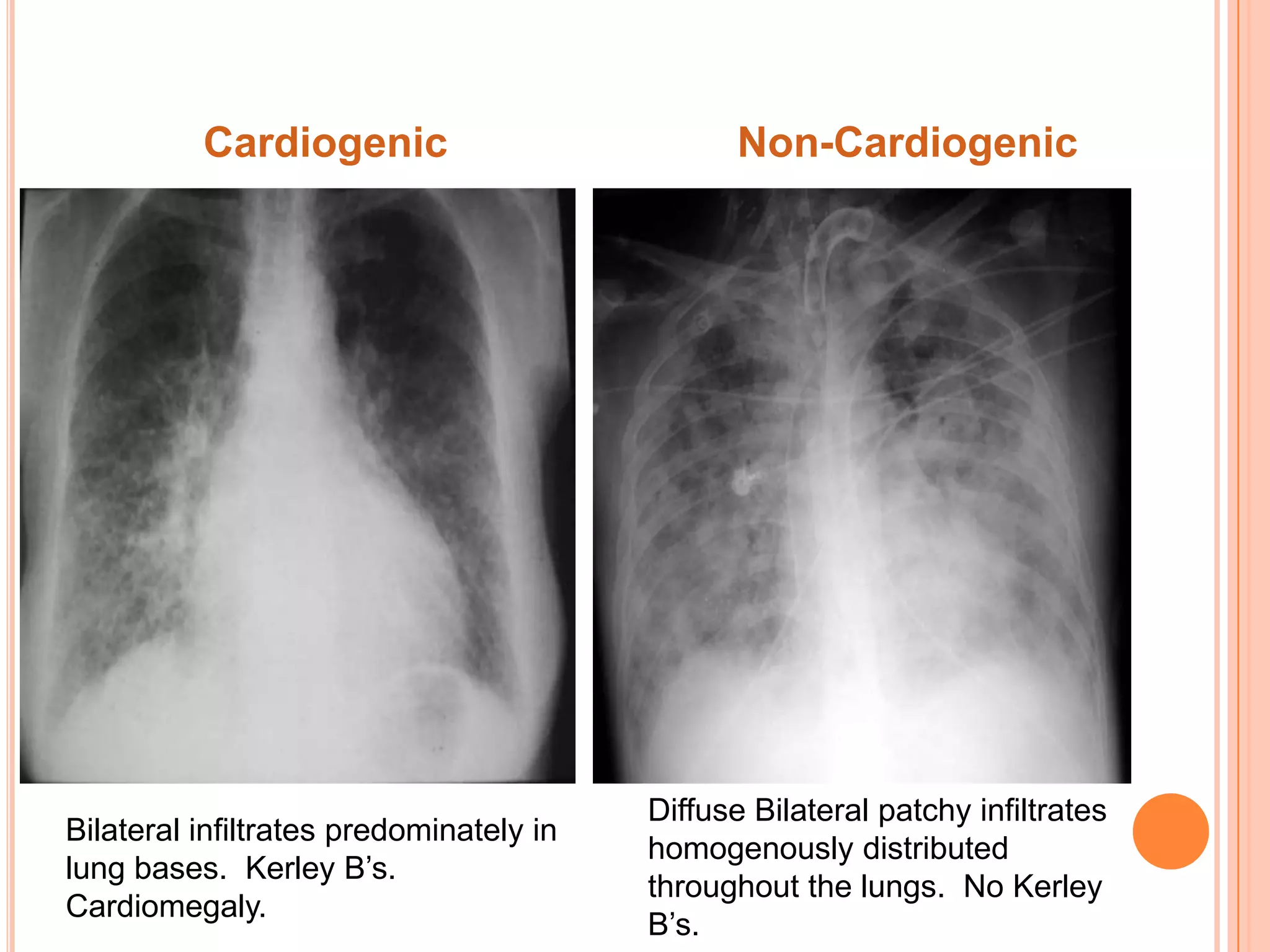
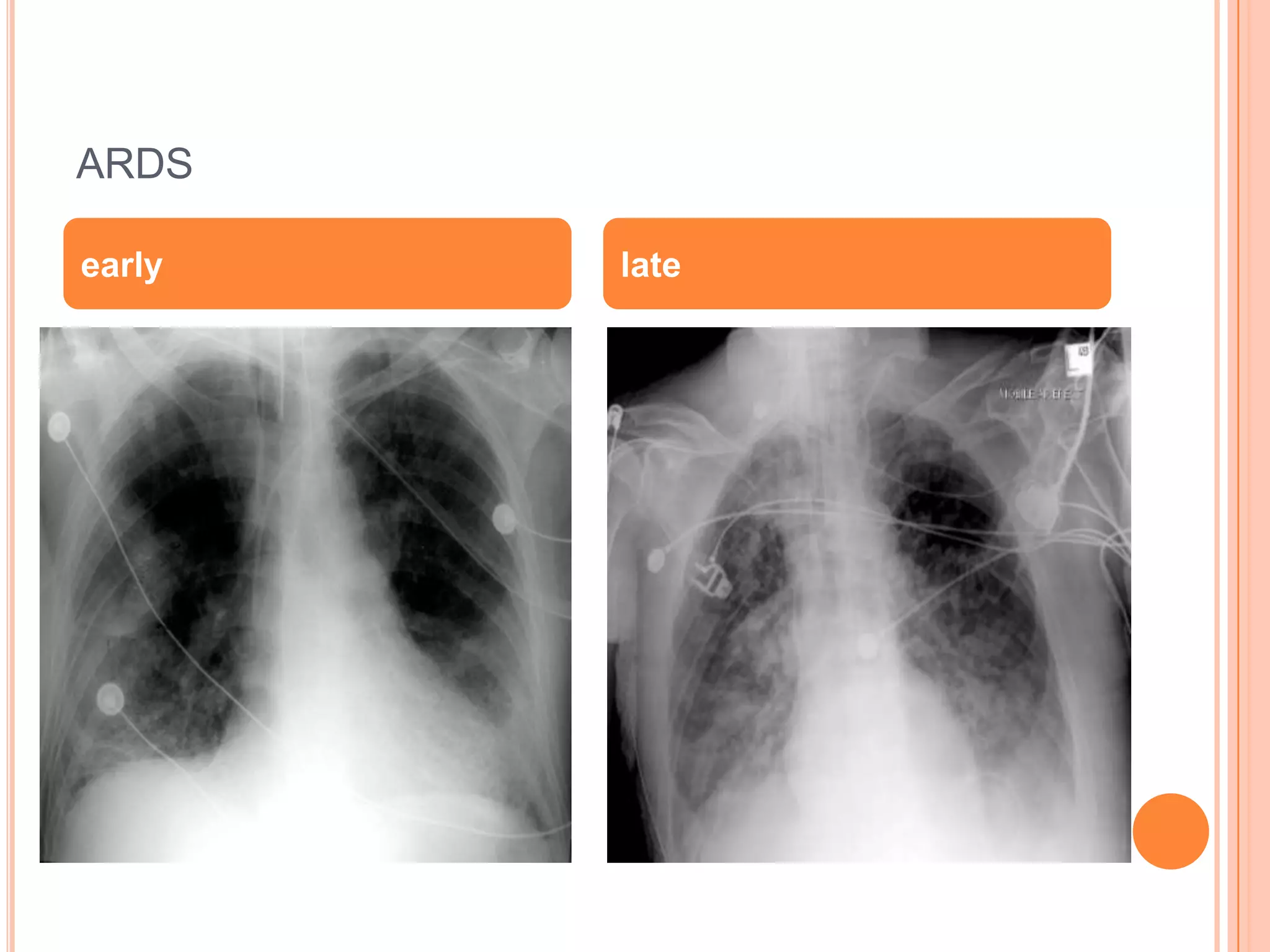
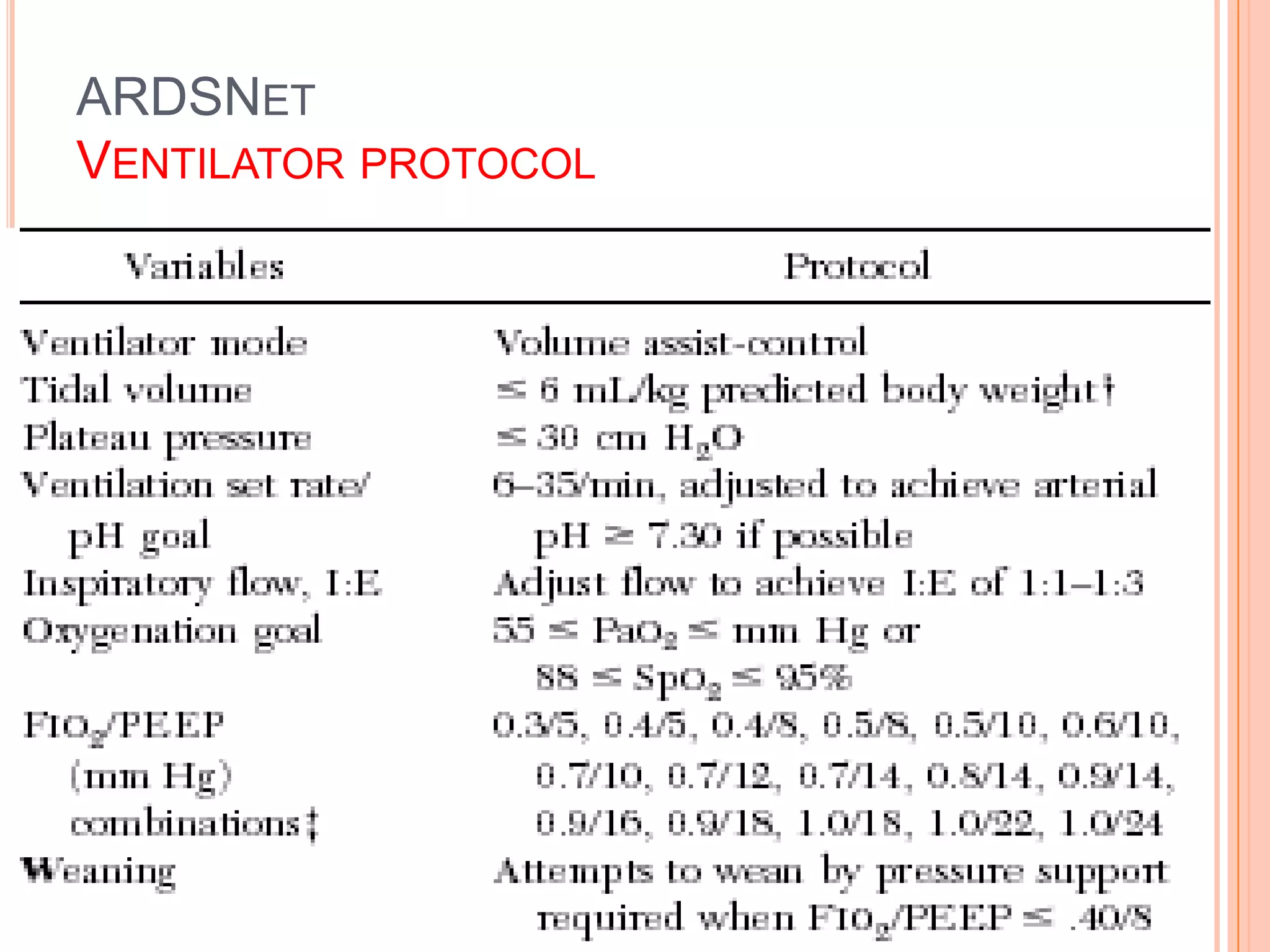
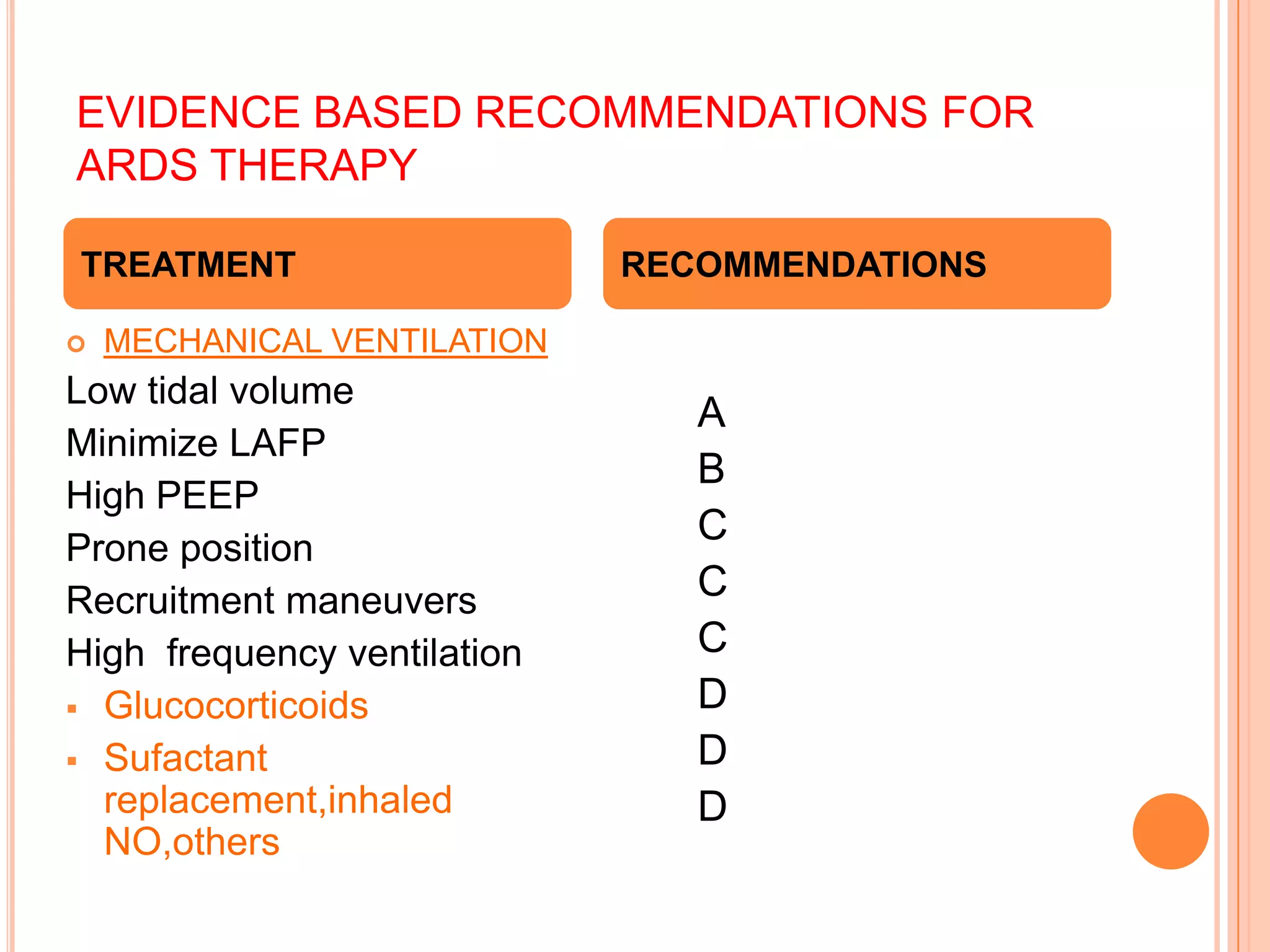
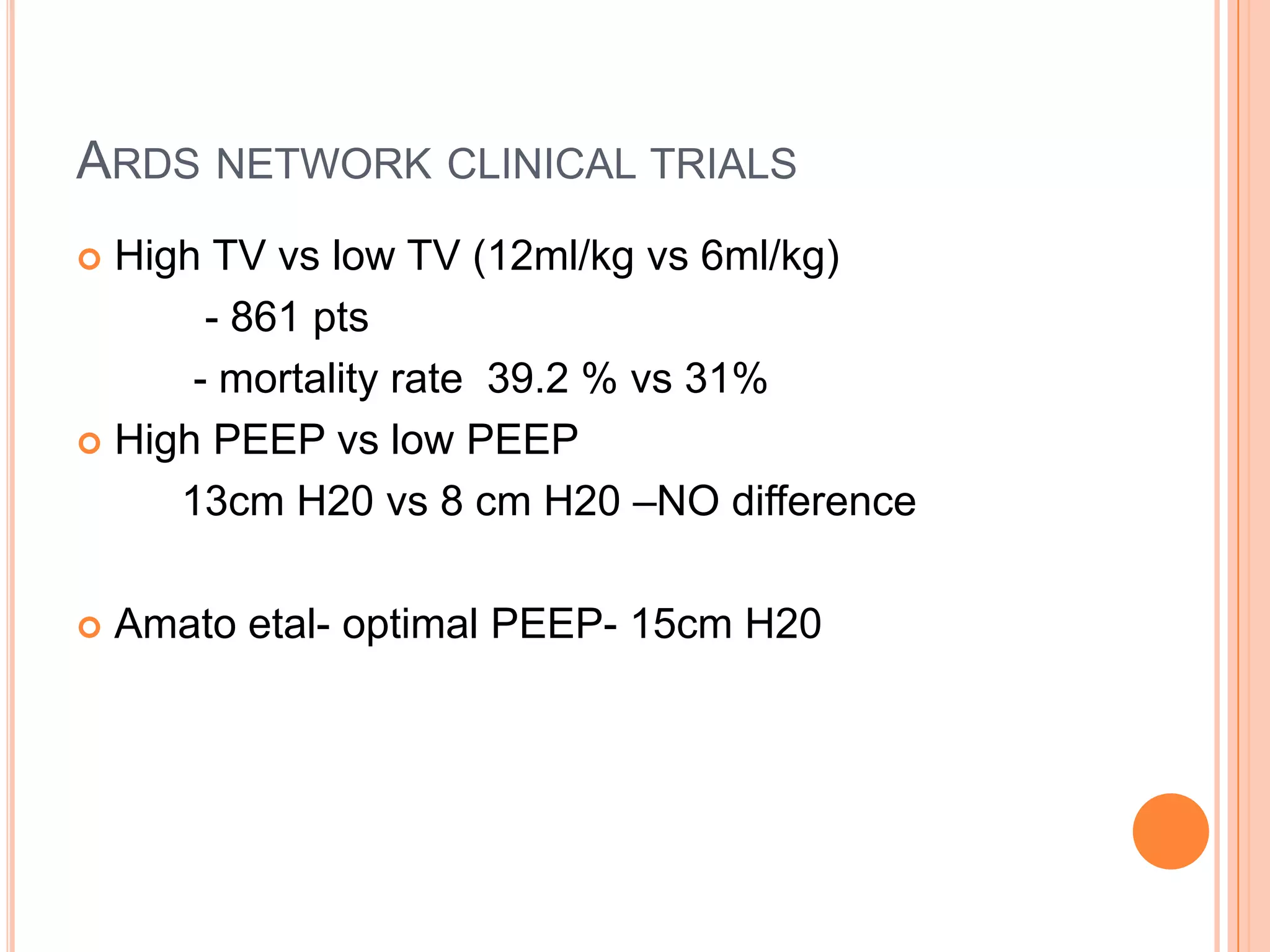
The document provides information about Acute Respiratory Distress Syndrome (ARDS) including its definition, pathophysiology, diagnosis, management, and prognosis. ARDS is defined as rapid onset hypoxemia and diffuse pulmonary infiltrates leading to respiratory failure. It is caused by direct lung injury from conditions like pneumonia or indirect injury from sepsis or trauma. Diagnosis involves criteria of acute onset, hypoxemia with PaO2/FiO2 ≤200, and no heart failure. Management focuses on treating the underlying cause and providing ventilator support using low tidal volumes per the ARDSNet protocol to reduce ventilator-induced lung injury. Prognosis depends on risk factors and mortality ranges from 26-44%.