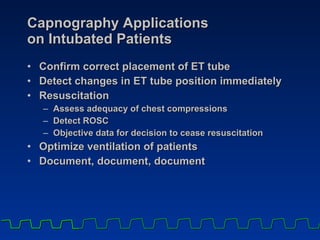
Capnography can be used to summarize 3 key applications for intubated patients:
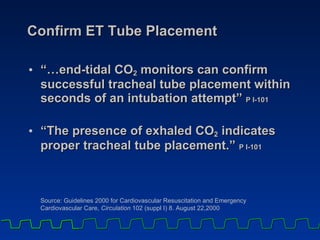
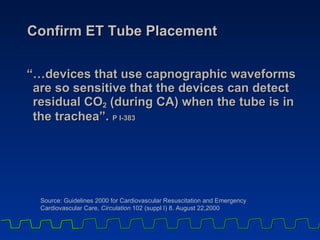
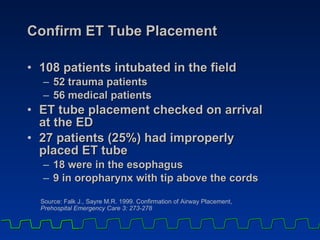
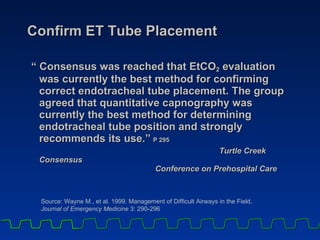
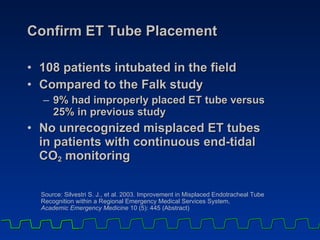
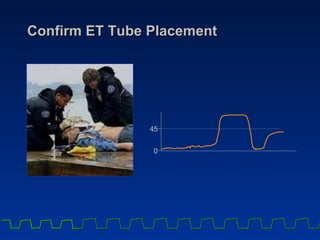
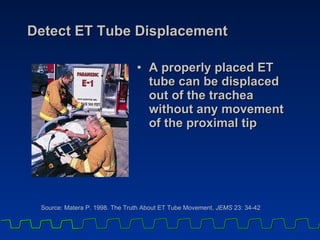
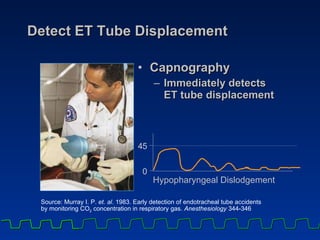
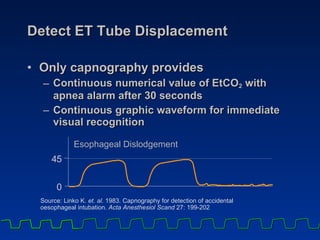
1) It can confirm correct endotracheal tube placement and detect displacement. Characteristic waveforms indicate proper vs displaced placement.
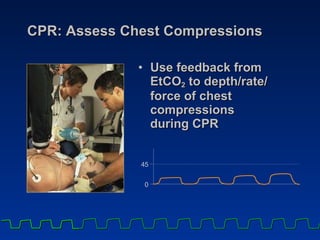
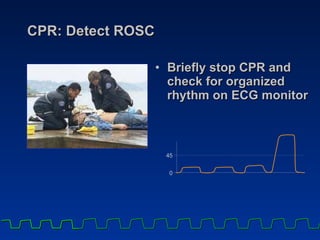
2) During CPR, it can assess the effectiveness of chest compressions by correlating end-tidal CO2 levels with cardiac output and blood flow.
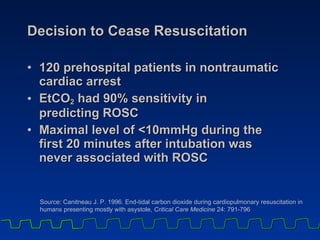
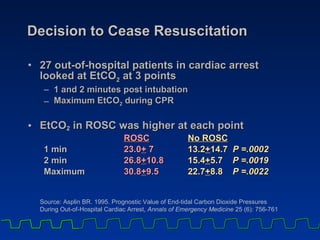
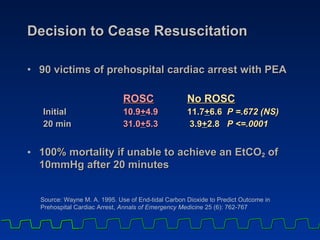
3) It provides an early indicator of return of spontaneous circulation through a rapid rise in CO2 levels, earlier than other signs like pulse or blood pressure. It also aids the decision to cease resuscitation efforts based on CO2 levels.