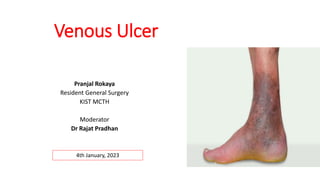
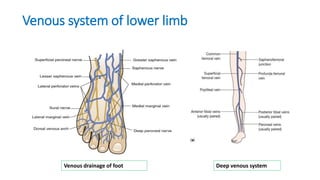
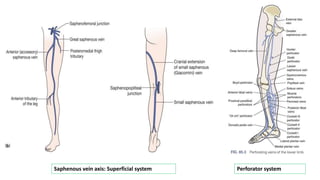
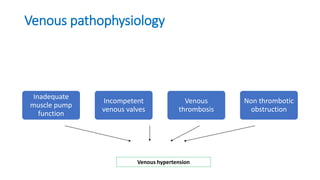
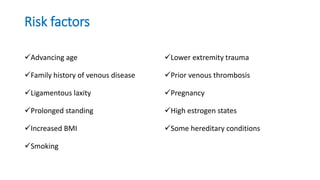
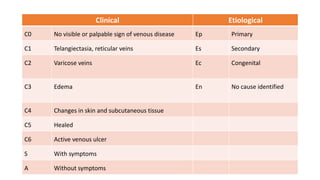
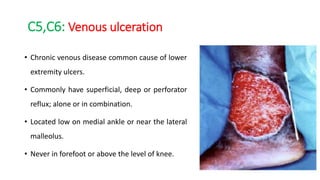
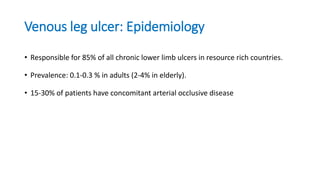
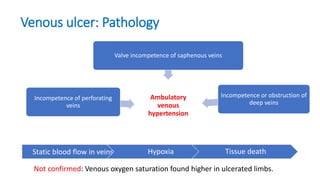
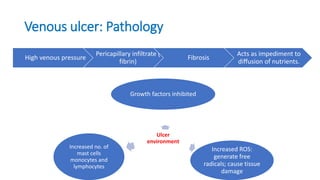
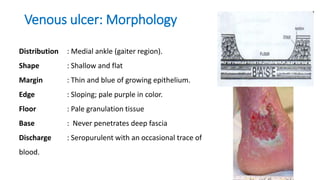
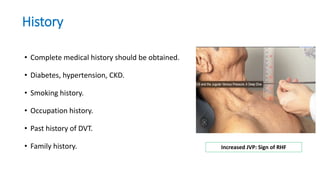
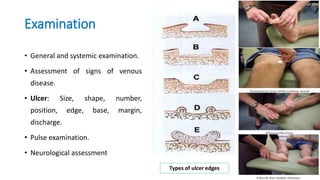
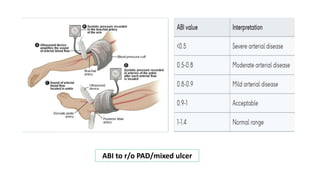
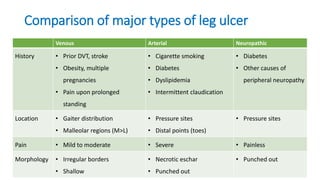
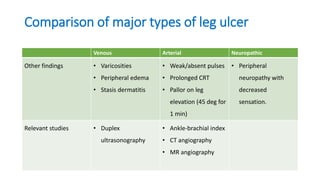
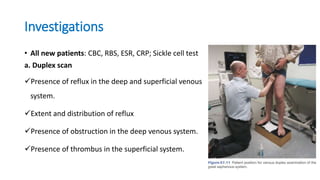
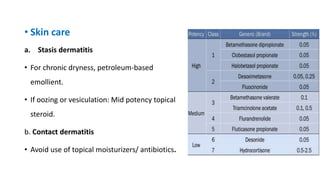
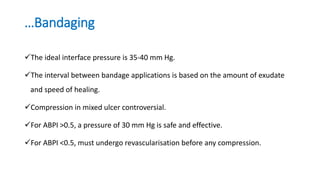
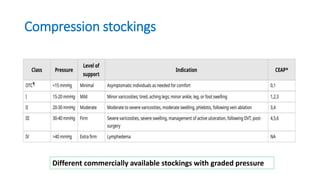
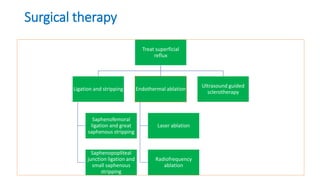
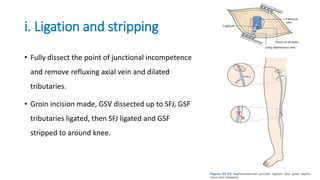
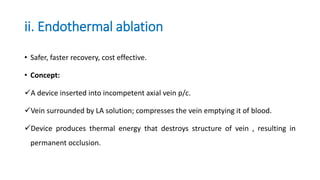
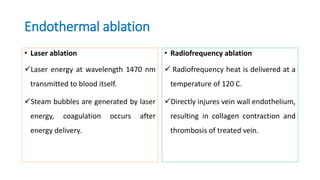
Venous ulcers are caused by venous hypertension due to incompetent valves in the veins of the lower leg. Risk factors include older age, family history, obesity, smoking, and prior deep vein thrombosis. Clinically, venous ulcers present as shallow wounds on the medial ankle that never penetrate deep tissue. Diagnosis involves assessing signs of venous insufficiency and duplex ultrasound to identify refluxing veins. Treatment focuses on compression therapy to reduce venous pressure along with wound care, pharmacotherapy, and sometimes surgical ablation of refluxing superficial veins to prevent recurrence. Prognosis is good for wound healing but recurrence rates remain high without continued compression.