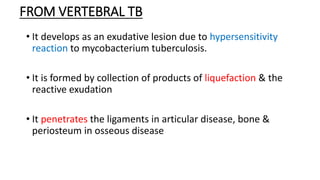
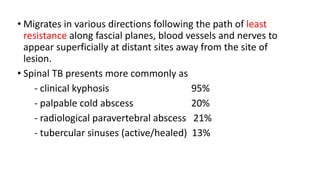
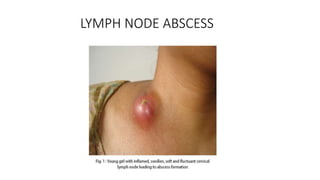
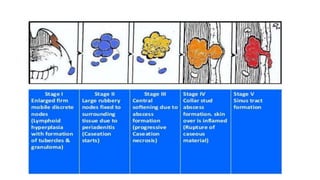
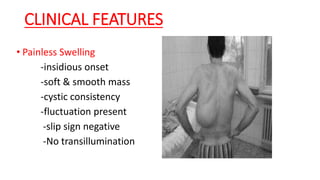
1) Cold abscesses are collections of pus that develop slowly without signs of inflammation and are usually caused by tuberculosis infection elsewhere in the body, commonly the lymph nodes or bones.
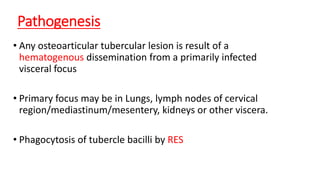
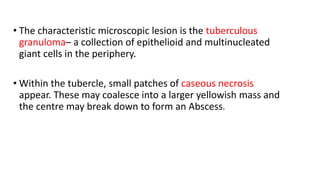
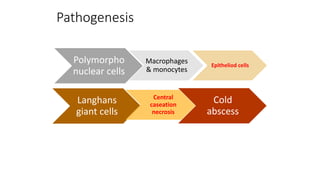
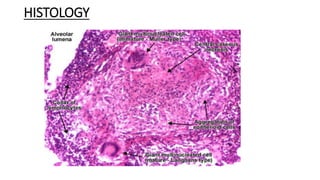
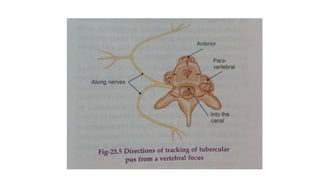
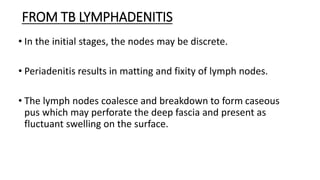
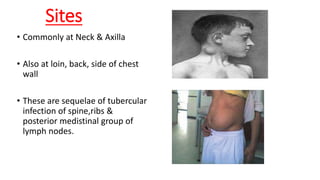
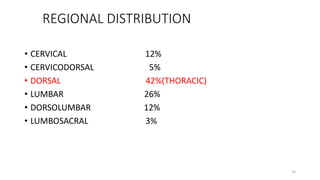
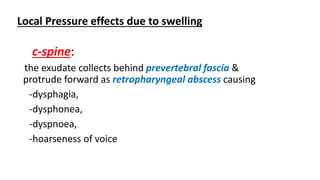
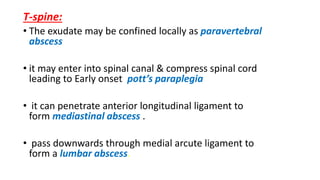
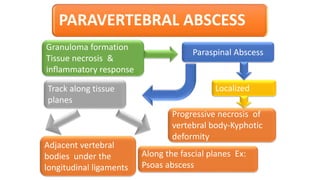
2) They form via a pathological process where the tuberculosis bacteria are phagocytosed by immune cells, forming granulomas with caseous necrosis that can break down and track along tissue planes, appearing as painless swellings distant from the original infection site.
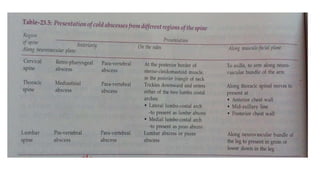
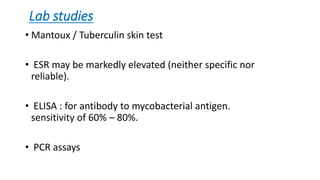
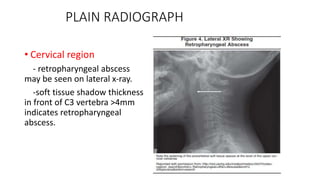
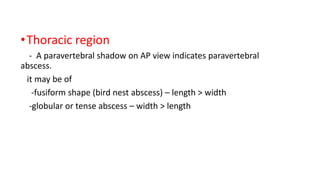
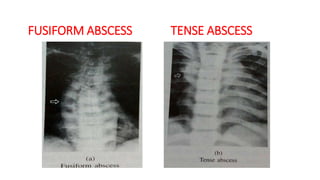
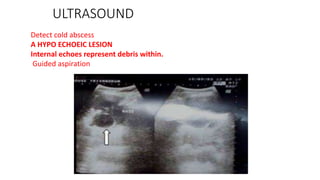
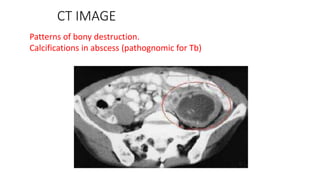
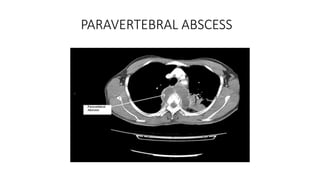
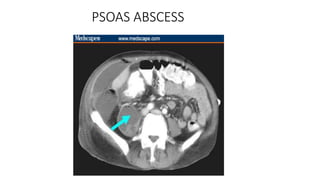
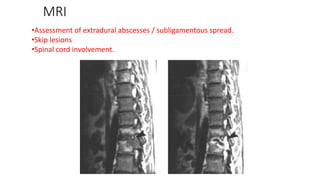
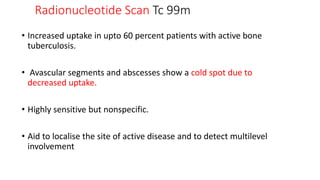
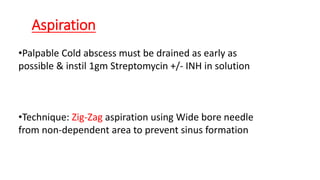
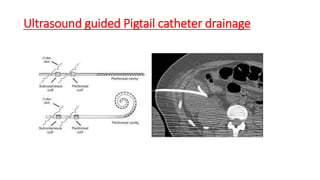
3) Diagnosis involves tuberculin skin testing, biopsy or aspiration of the abscess, and radiological imaging like ultrasound or CT scan may help locate the abscess. Treatment consists of anti-tuberculosis drugs alongside drainage of palpable abscesses.