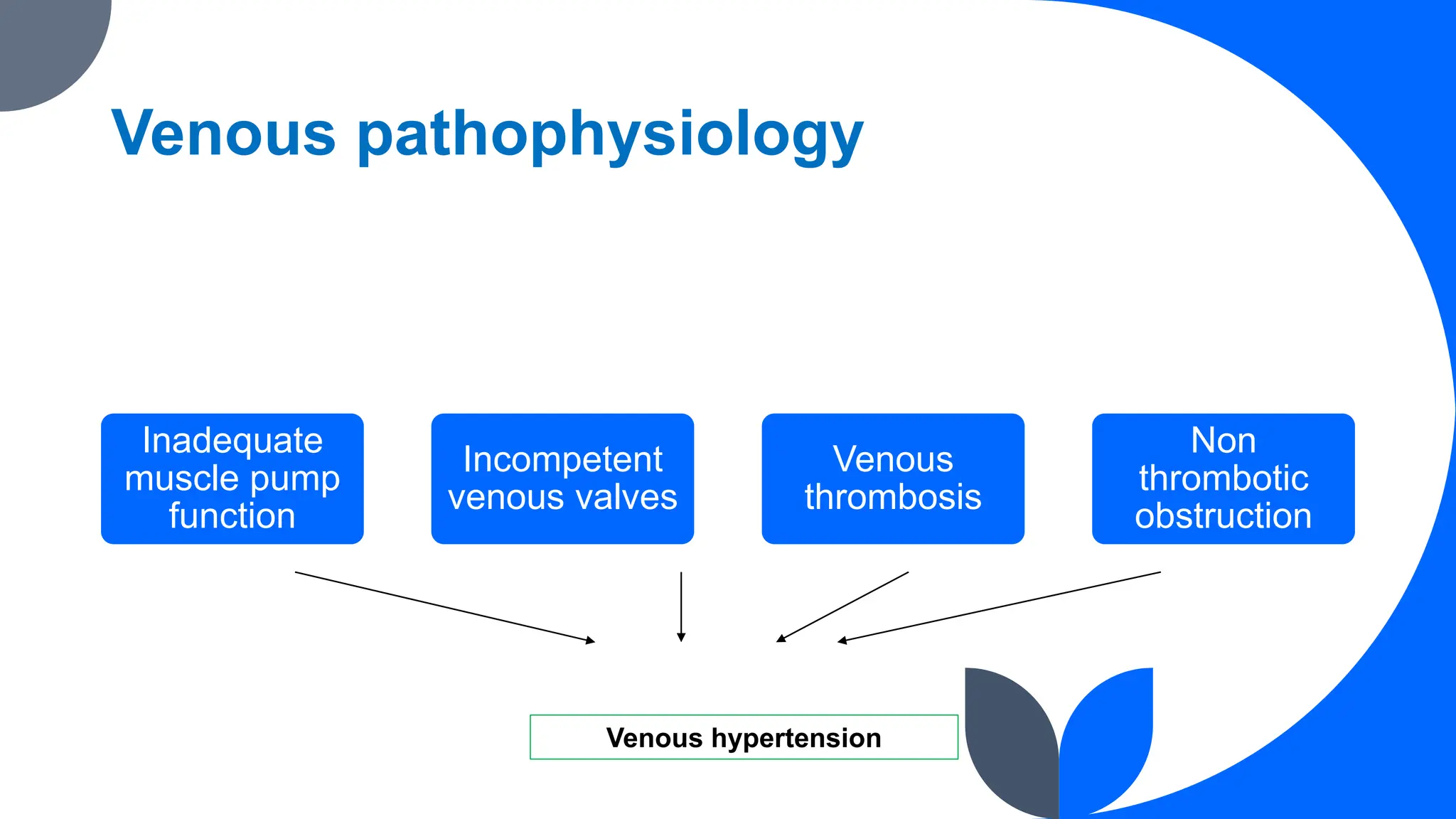
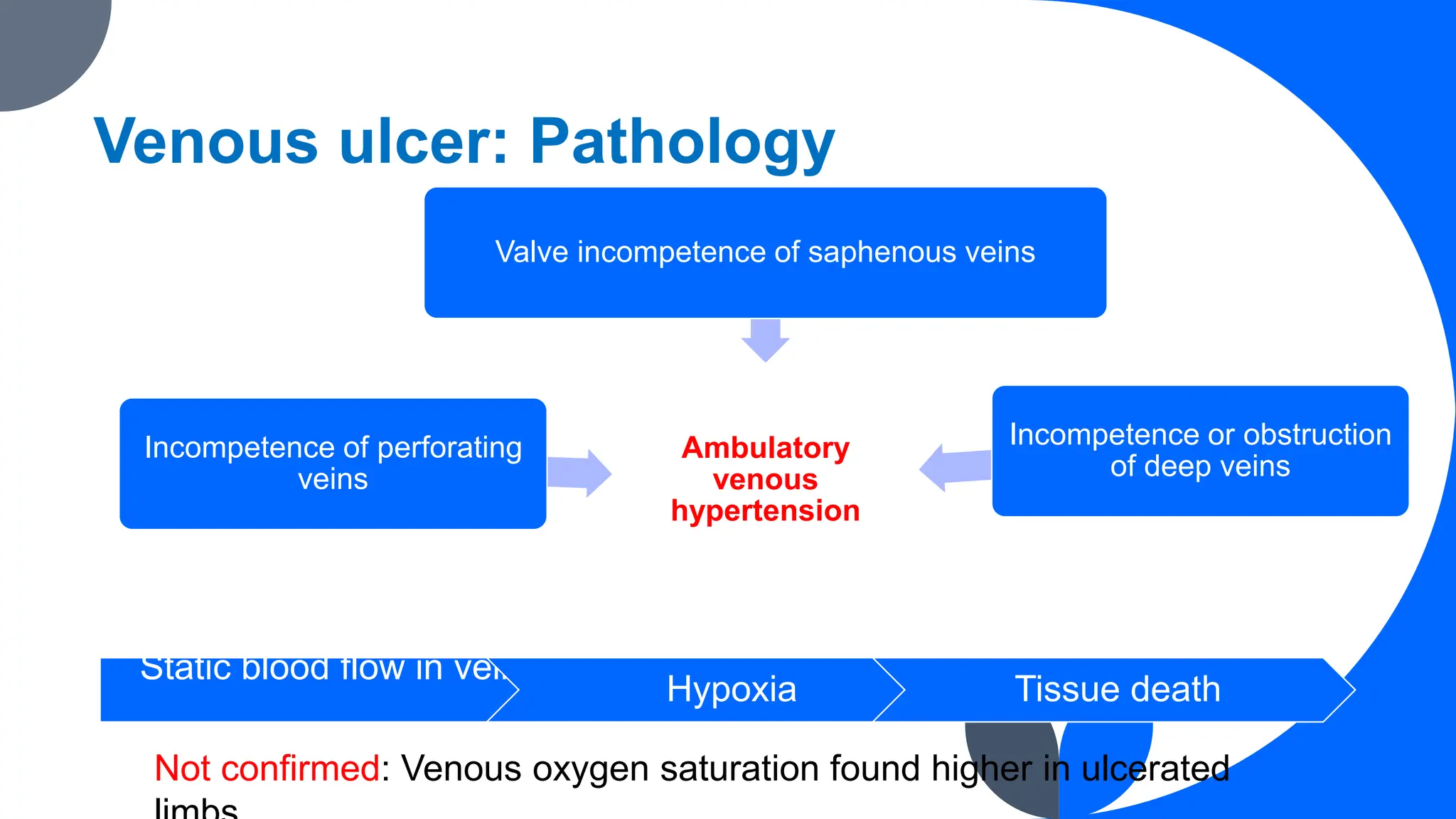
Chronic venous insufficiency (CVI) results from persistent venous hypertension leading to various clinical symptoms, including edema and ulcers. Common causes include age, heredity, and prolonged standing, with management focusing on compression therapy and surgical options when necessary. Diagnosis may involve duplex ultrasound, and the classification of venous disease is often guided by the CEAP system.