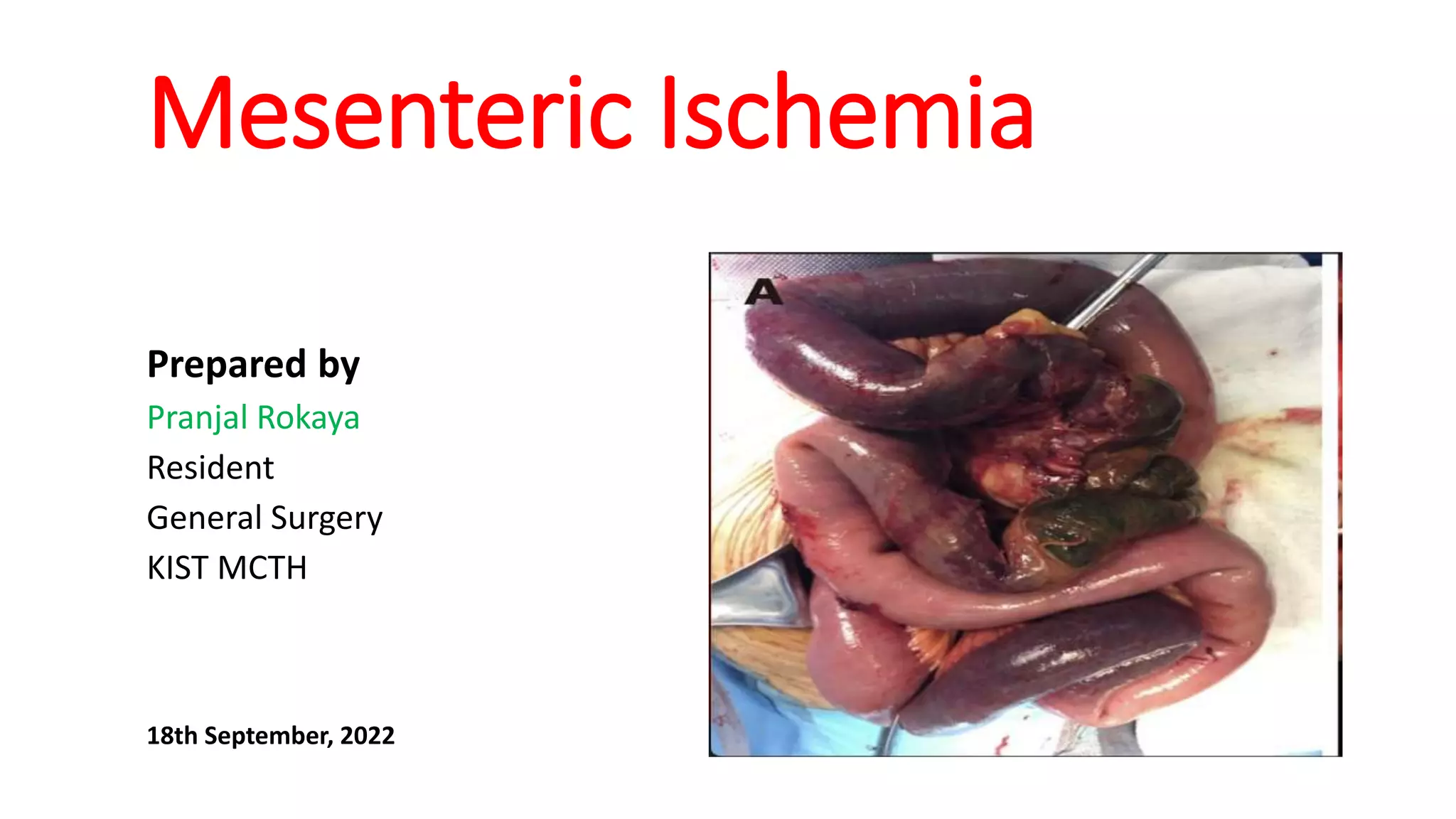
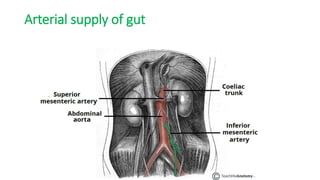
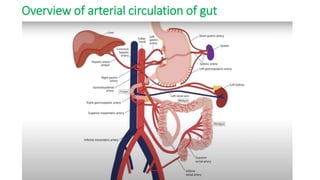
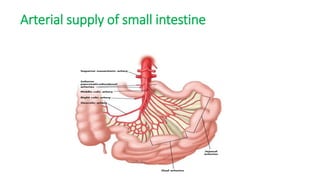
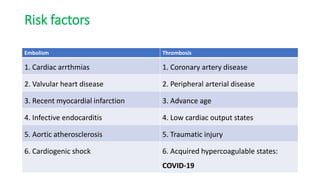
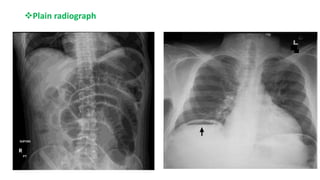
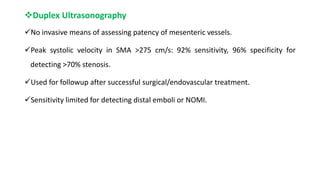
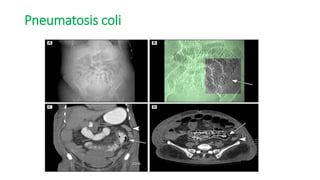
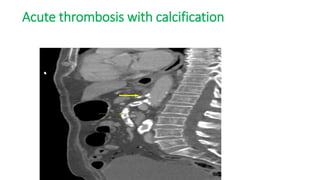
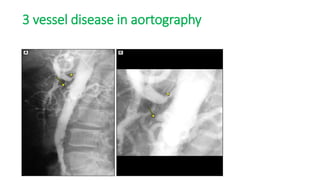
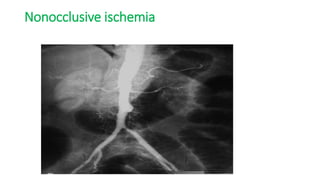
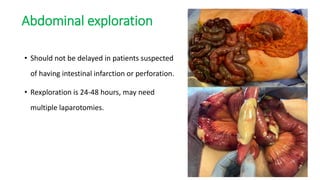
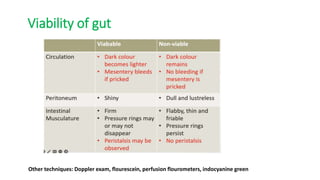
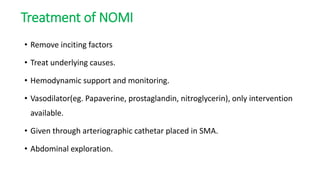
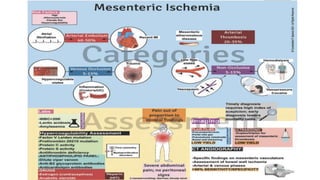
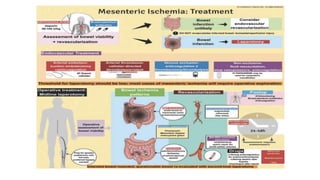
This document provides an overview of mesenteric ischemia, including its various types, risk factors, clinical features, diagnosis, and management. It begins with definitions of relevant terms like ischemia, infarction, embolism, and thrombosis. It then describes the different types of mesenteric ischemia - acute, chronic, and non-occlusive. For each type, it outlines typical causes, risk factors, clinical presentations, diagnostic approaches, and treatment options, which may involve endovascular or open surgical revascularization procedures. It concludes by noting the generally poor prognosis of acute mesenteric ischemia but improved outcomes with timely diagnosis and treatment.