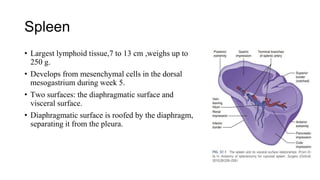
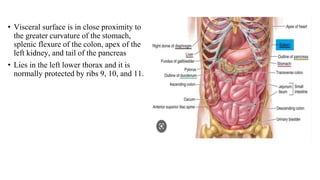
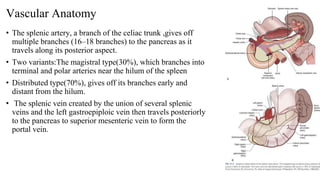
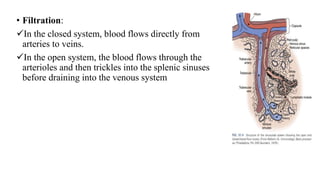
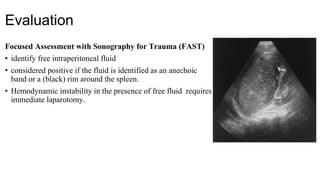
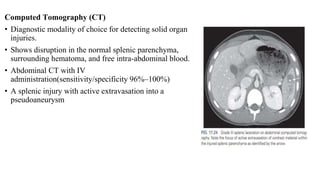
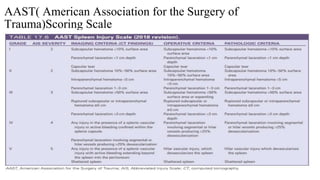
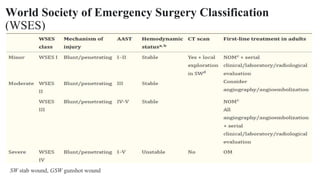
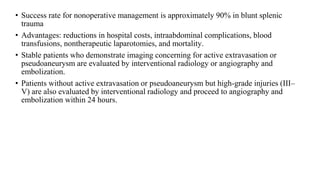
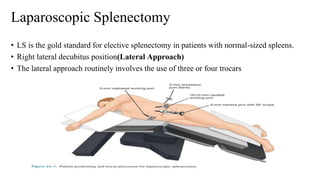
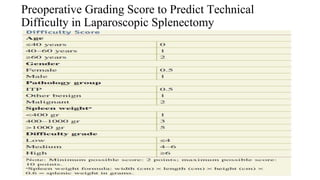
This document provides an overview of the spleen, splenic injuries, and approaches to splenic surgery. It describes the spleen's anatomy, vascular supply, functions, and types of injuries. For splenic injuries, it discusses evaluation with FAST and CT scans, injury grading scales, and management approaches like angiography, embolization, splenorrhaphy versus splenectomy. It then covers surgical techniques for open and laparoscopic splenectomy, including positioning, mobilization, hilar dissection and hemostasis. Postoperative risks are also summarized.