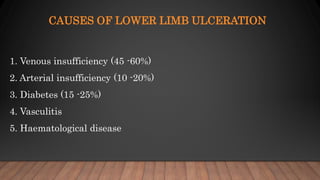
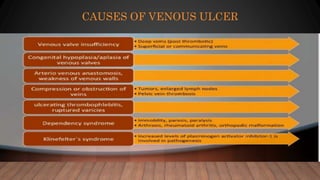
1) Venous ulcers are caused by venous insufficiency and often occur on the lower medial aspect of the leg.
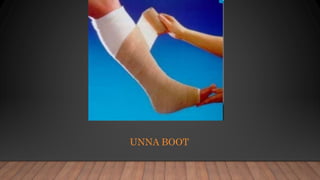
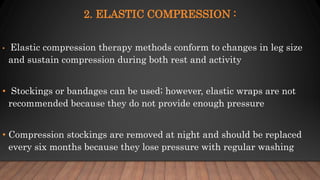
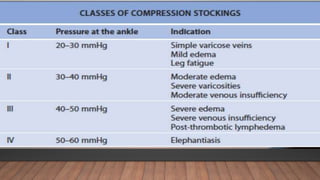
2) Compression therapy is the standard treatment to reduce edema and enhance healing. Elastic compression stockings are recommended.
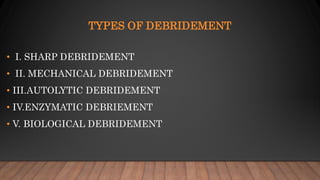
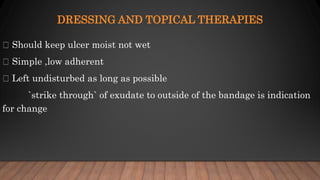
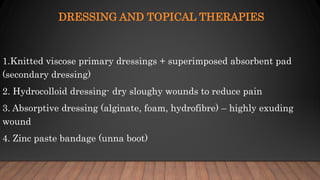
3) Debriding and dressing the wound along with treating underlying causes such as varicose veins or eczema also aids healing.
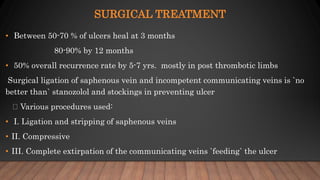
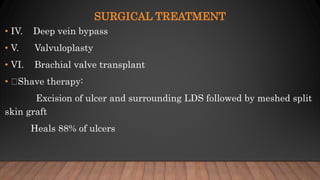
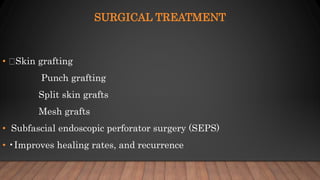
4) Surgery to remove incompetent veins may be considered if conservative measures fail to heal the ulcer. Lifelong compression is still needed after healing to prevent recurrence.