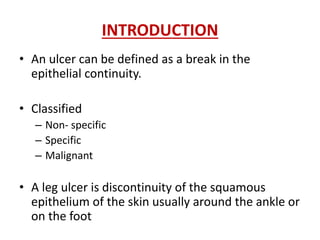
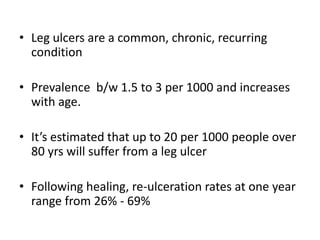
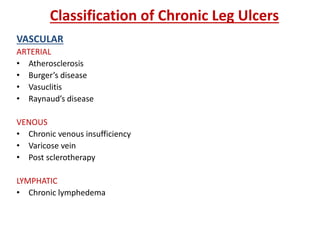
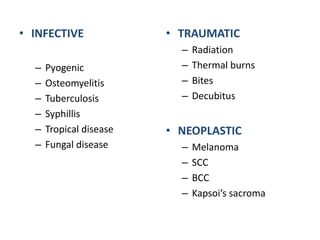
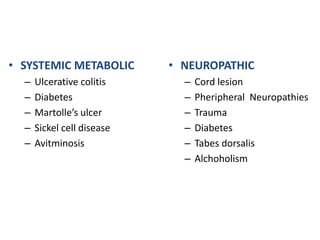
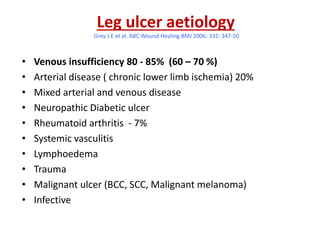
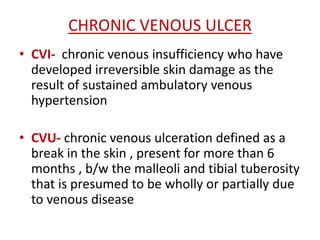
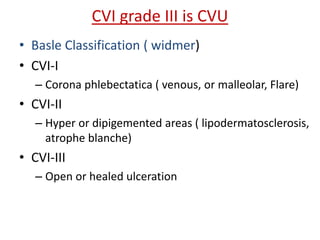
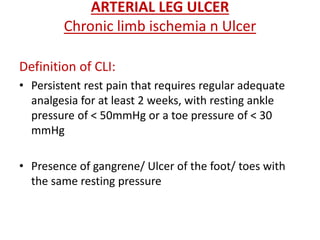
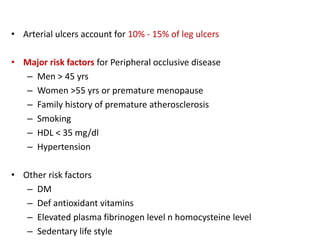
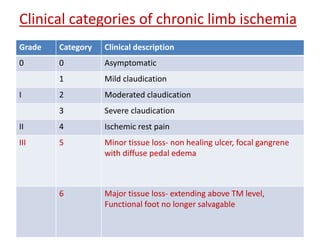
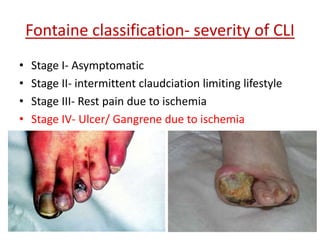
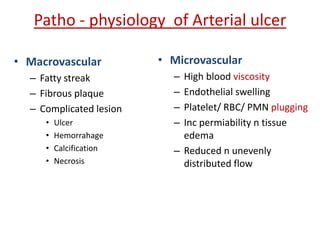
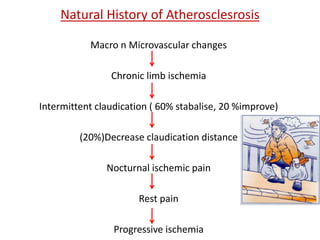
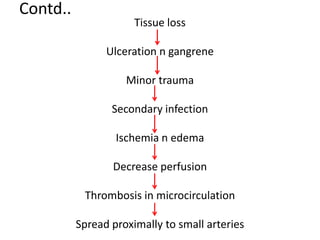
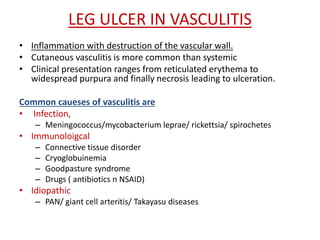
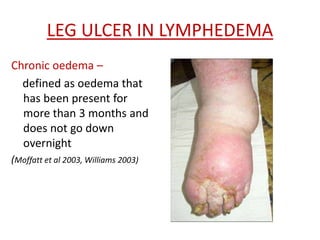
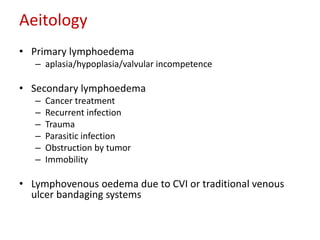
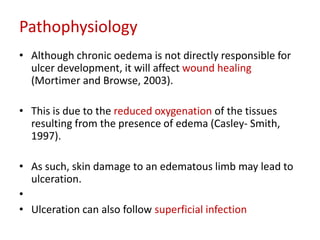
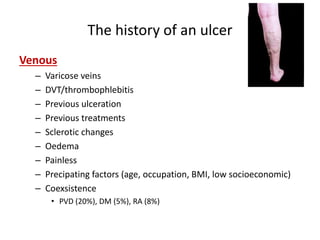
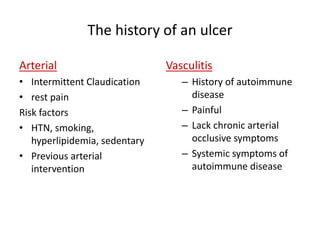
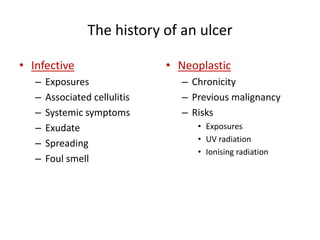
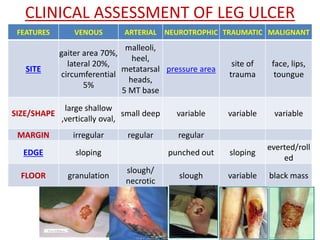
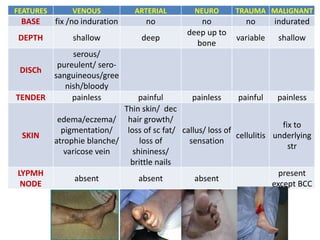
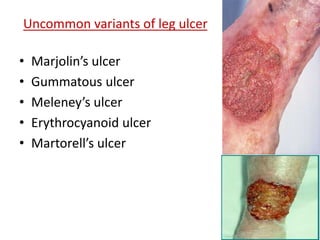
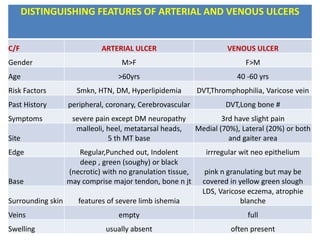
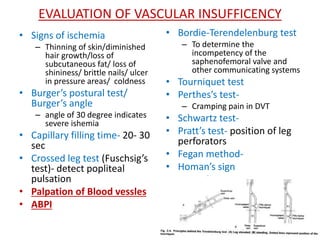
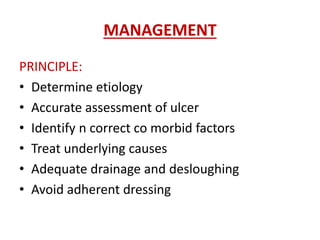
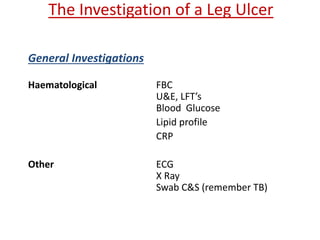
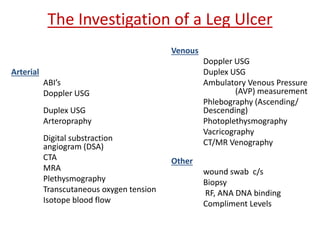
The document discusses the approach and classification of leg ulcers. It begins by defining a leg ulcer and classifying them as non-specific, specific, or malignant. The main causes of leg ulcers are then discussed, including venous insufficiency (80-85% of cases), arterial disease, neuropathy, infection, trauma, and malignancy. Diagnostic evaluation of a leg ulcer involves obtaining a thorough history and physically examining the ulcer, surrounding skin, and vascular and neurological systems. Key distinguishing features of venous versus arterial ulcers are also provided.