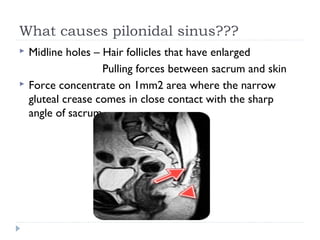
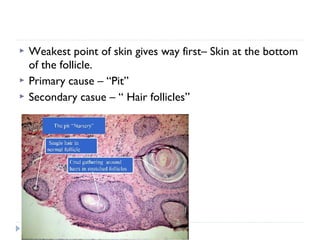
Pilonidal sinus is an infection of the skin and subcutaneous tissue near the upper part of the natal cleft. It is caused by hair penetrating and becoming trapped in the skin. Surgical excision is often required for chronic cases. Primary closure has faster healing but higher recurrence, while delayed closure has slower healing but lower recurrence. Off-midline primary closure has better outcomes than midline with respect to time to heal, infections, and recurrence rates. Lateral advancement flaps like Karydakis have shown slightly better results than Limberg flaps for off-midline closure. Antibiotics generally only have a role if cellulitis is present.






















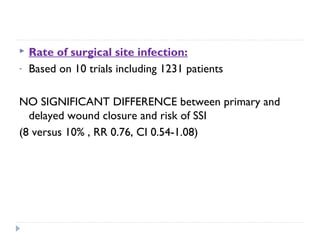
![ Recurrence rates:
- Based on 16 trials including 1666 patients , the overall
recurrence rate was 6.9%.
- Primary wound closure was associated with a HIGHER
recurrence rate compared to delayed wound closure.
(8.7 versus 5.3 percent, relative risk RR [1.5] CI1.08-2.17](https://image.slidesharecdn.com/pilonidalsinus-150422085043-conversion-gate02/85/Pilonidal-sinus-32-320.jpg)