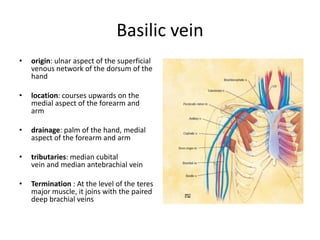
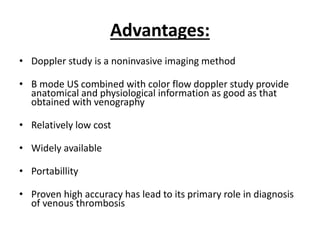
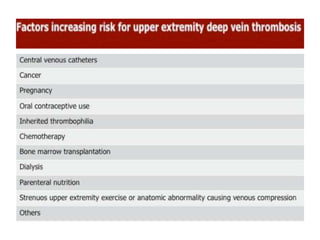
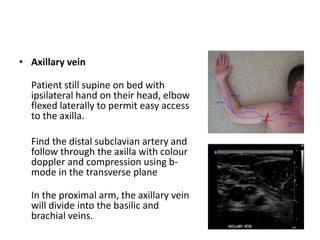
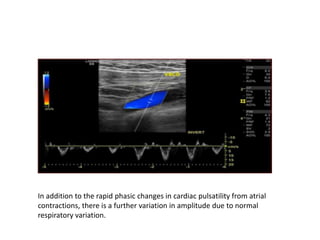
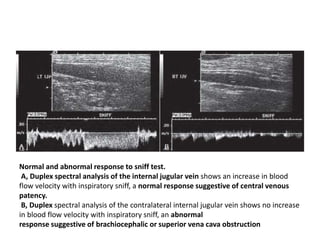
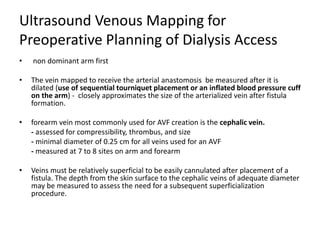
This document discusses the anatomy and ultrasound evaluation of veins in the upper extremity. It describes the cephalic, basilic, brachial, axillary, subclavian, and internal jugular veins. The technical procedure for venous doppler ultrasound is outlined, including patient positioning, scanning techniques, and diagnostic criteria. Potential pitfalls like rouleaux and limited windows are noted. Chronic changes after deep vein thrombosis like valve changes and collateral veins are also described. Ultrasound is useful for evaluating suspected deep vein thrombosis and mapping veins for dialysis access planning.