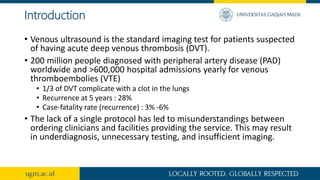
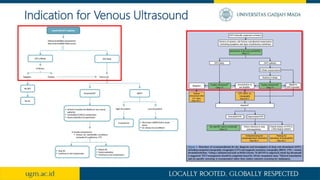
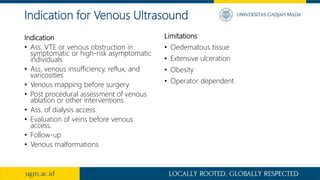
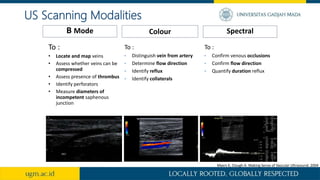
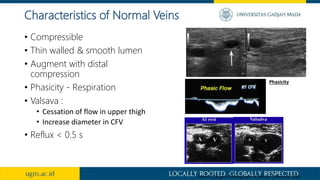
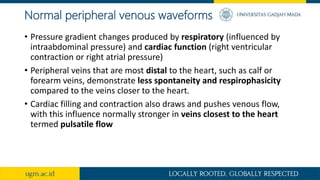
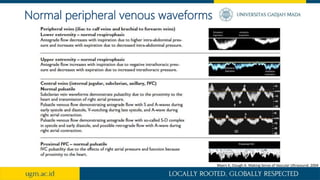
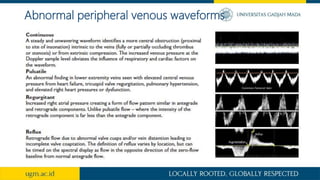
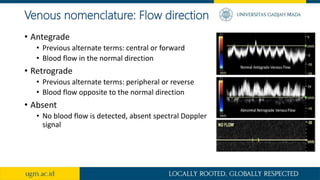
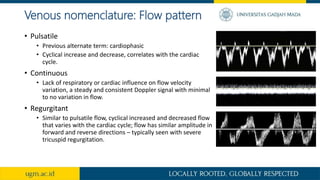
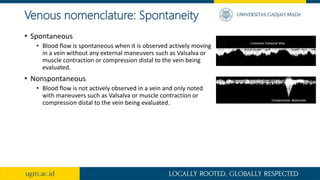
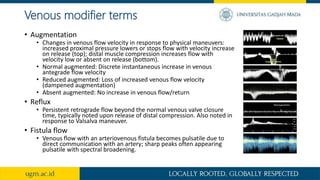
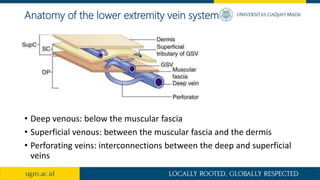
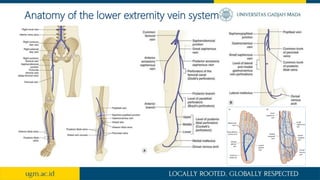
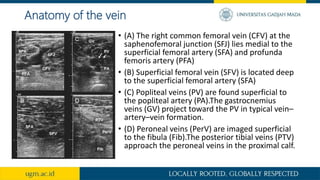
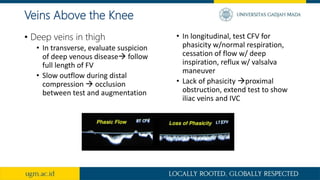
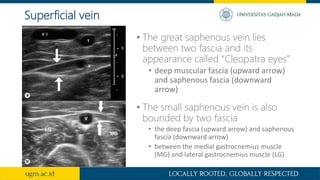
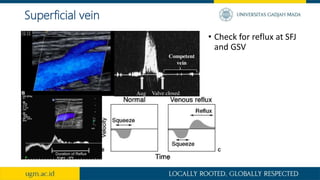
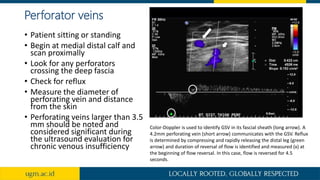
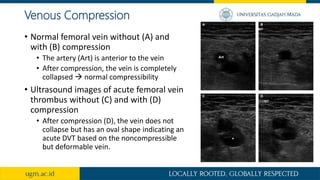
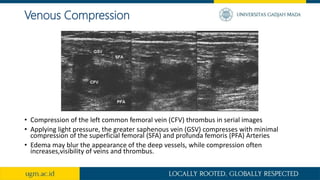
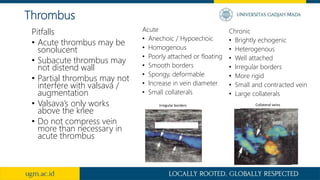
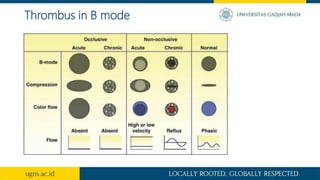
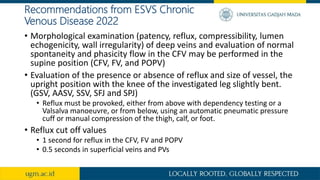
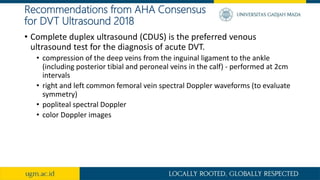
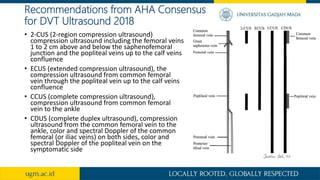
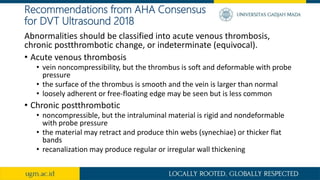
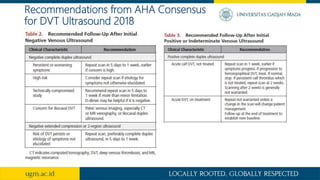
This document provides an overview of peripheral venous Doppler ultrasound of the lower extremities. It discusses the indications for venous ultrasound including evaluation of deep vein thrombosis, venous insufficiency, and pre-operative mapping. Normal venous ultrasound findings such as compressibility and phasicity are described. Abnormal findings of acute and chronic deep vein thrombosis are also outlined. The document reviews scanning techniques for different areas of the lower extremity veins and describes how to evaluate for reflux and thrombus. Recommendations from clinical guidelines on performing a complete venous ultrasound exam and classifying ultrasound findings are also summarized.