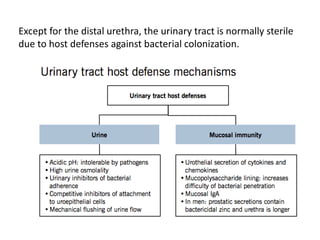
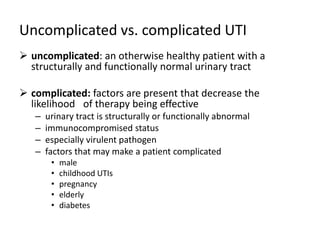
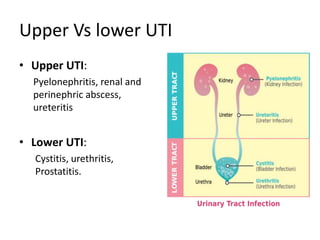
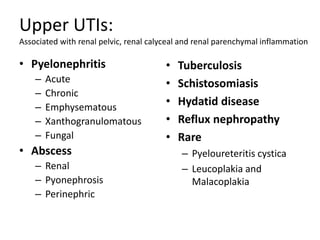
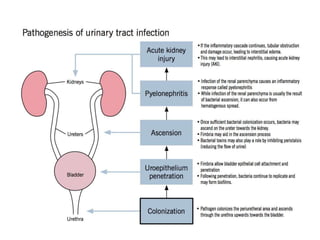
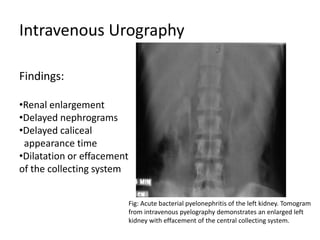
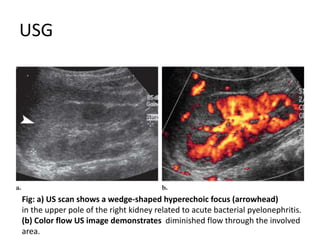
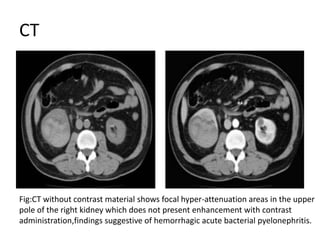
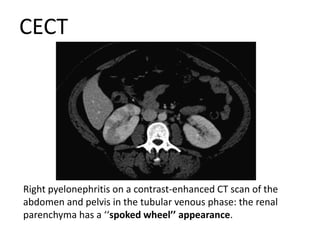
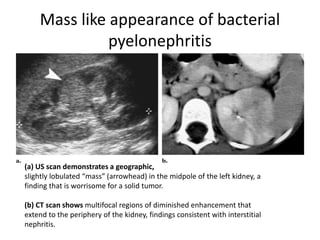
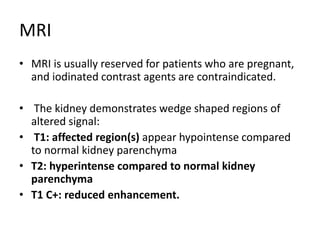
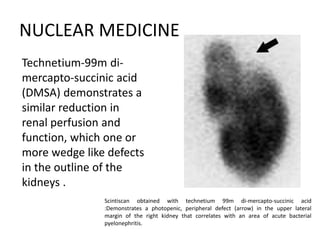
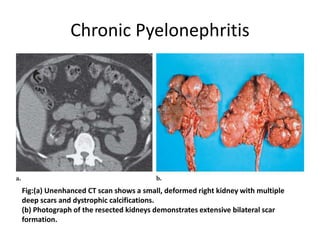
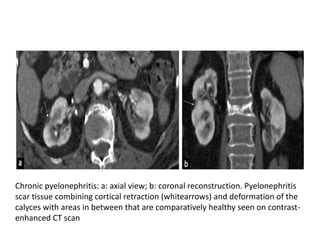
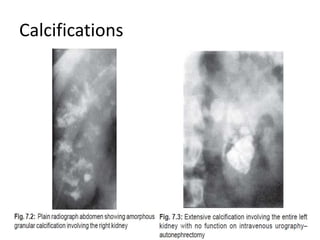
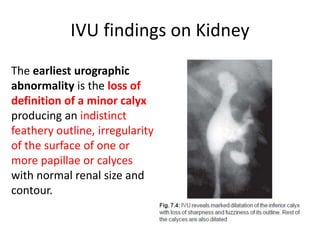
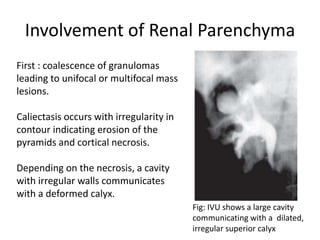
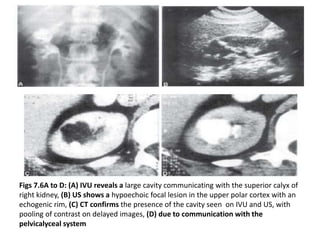
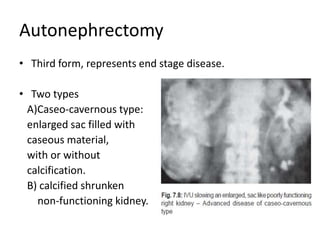
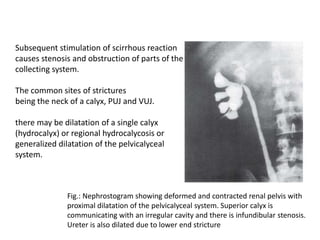
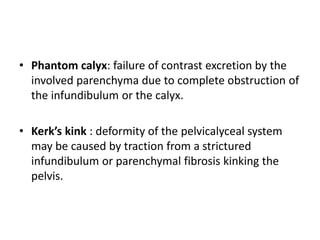
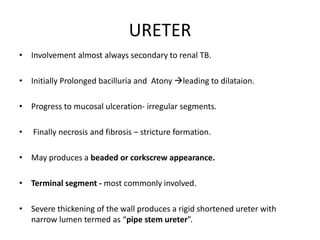
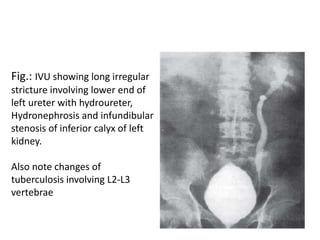
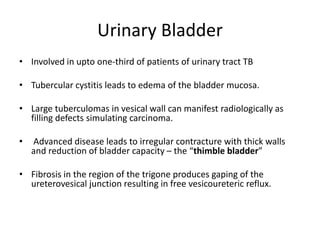
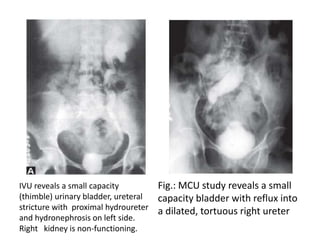
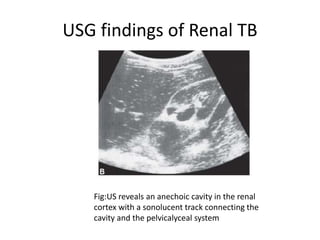
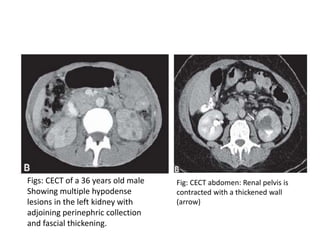
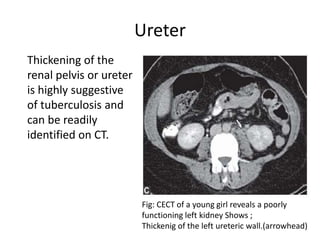
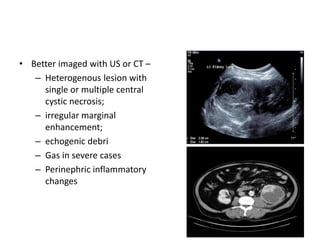
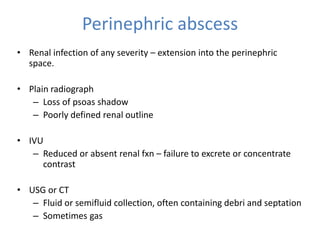
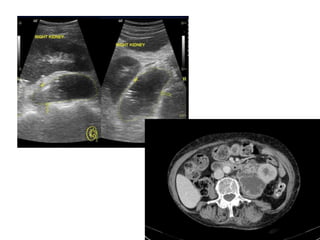
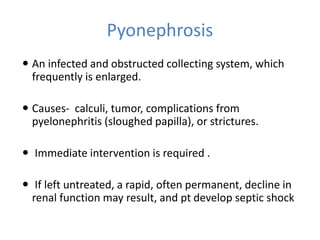
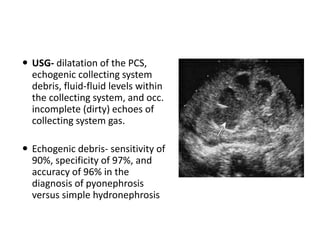
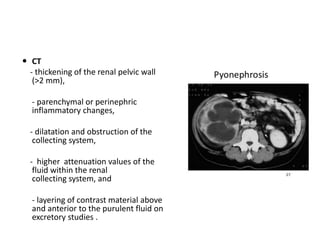
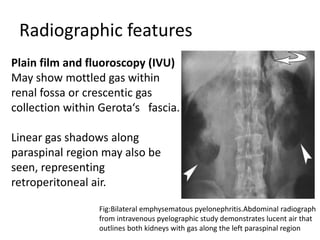
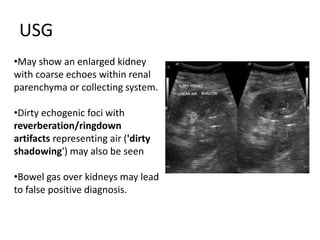
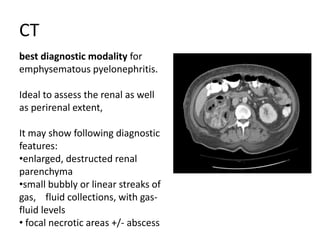
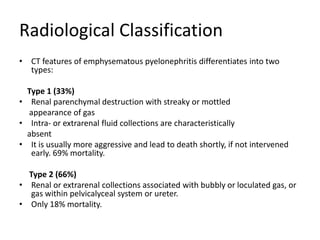
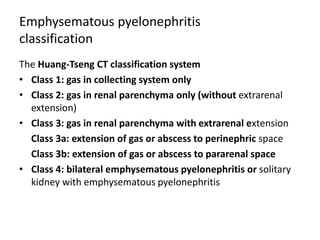
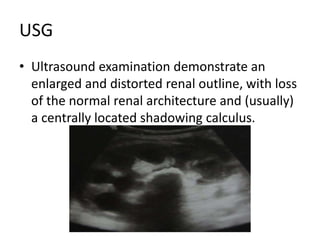
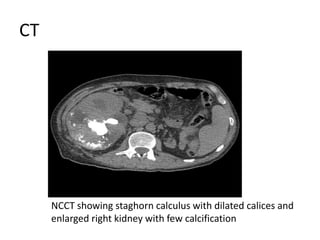
The document discusses radiological approaches to diagnosing and evaluating urinary tract infections (UTIs). It begins by distinguishing between upper and lower UTIs, as well as uncomplicated and complicated UTIs. Common causative organisms of UTIs are also identified. Various imaging modalities are then described for evaluating UTIs, including intravenous urography, ultrasound, CT, MRI, and nuclear medicine scans. Specific radiological findings of acute bacterial pyelonephritis, chronic pyelonephritis, tuberculous infections of the urinary tract are also summarized.