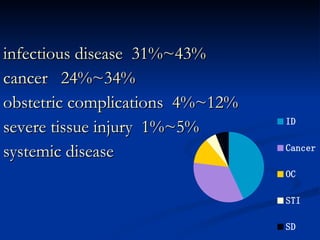
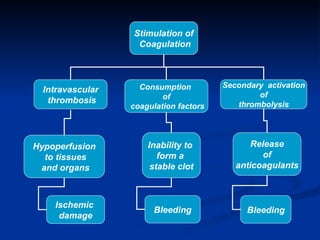
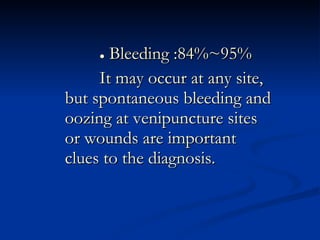
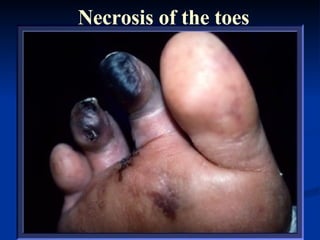
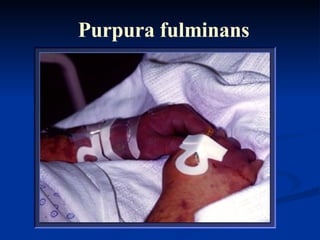
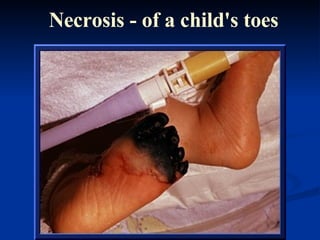
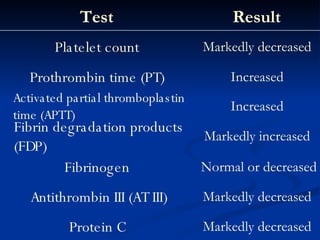
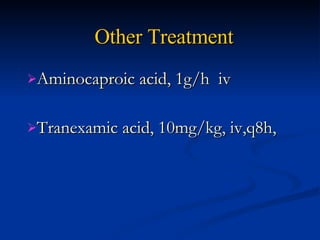
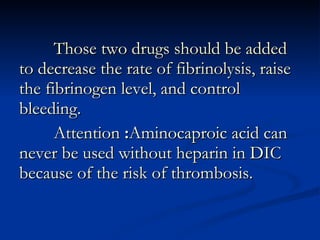
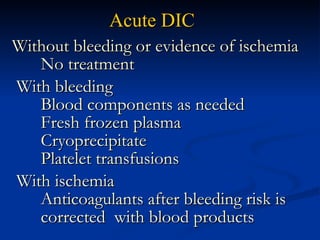
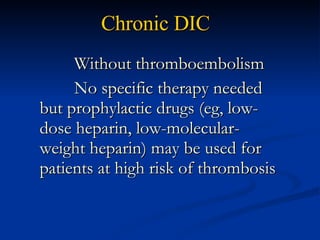
Disseminated intravascular coagulation (DIC) is a syndrome characterized by widespread activation of coagulation that can occur as a result of various underlying conditions. It results from an imbalance between coagulation and anticoagulation processes in the body. DIC can be acute, with bleeding and shock being dominant symptoms, or chronic, where thrombosis and clotting may predominate. The most common triggers of DIC are infectious diseases, cancer, obstetric complications, and severe tissue injury. Diagnosis involves identifying symptoms of bleeding and thrombosis, abnormal laboratory coagulation test results, and ruling out other conditions. Treatment focuses on treating the underlying cause, replacing coagulation factors, platelets, and fibrinogen, and