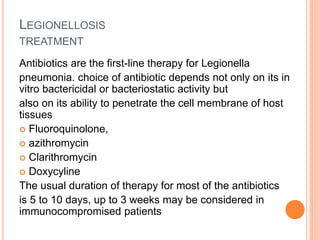
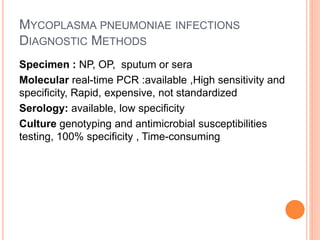
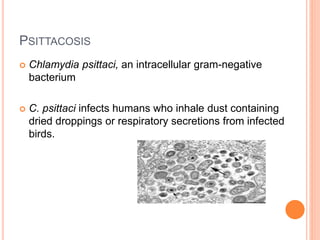
Atypical pneumonia is caused by certain bacteria including Mycoplasma pneumoniae, Chlamydia pneumoniae, Chlamydia psittaci, and Legionella pneumophila. It tends to cause milder symptoms than typical pneumonia and does not usually require hospitalization. Different antibiotics are required to treat atypical versus typical pneumonia. Common symptoms include a persistent cough, headache, and low-grade fever.