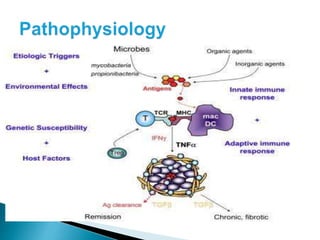
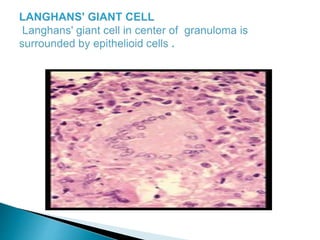
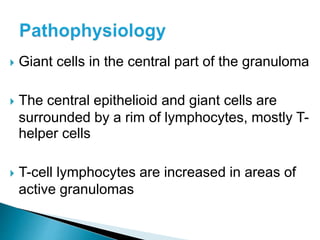
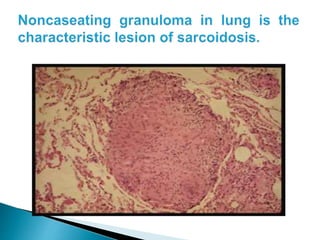
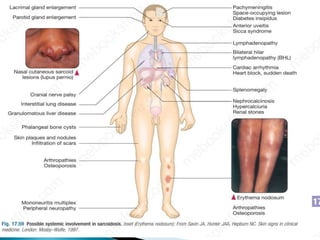
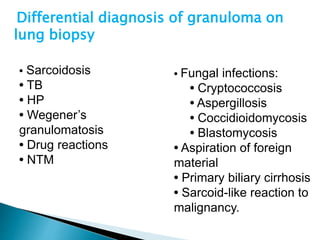
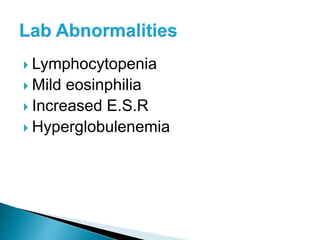
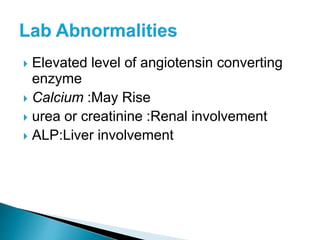
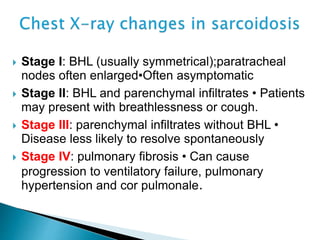
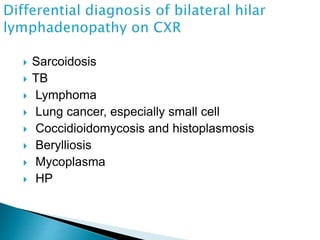
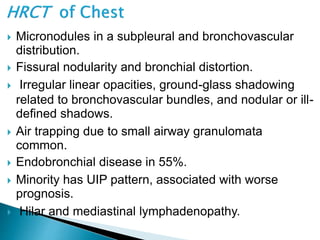
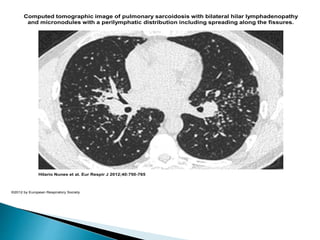
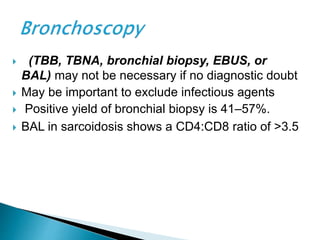
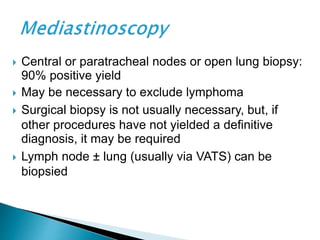
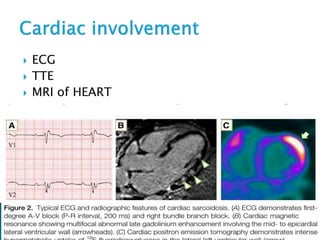
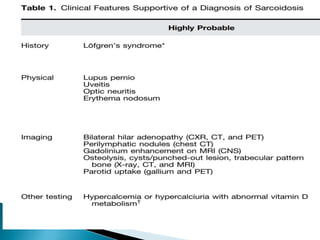
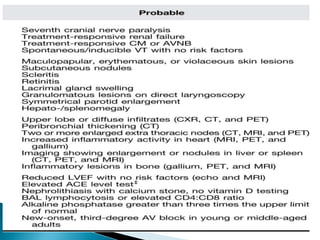
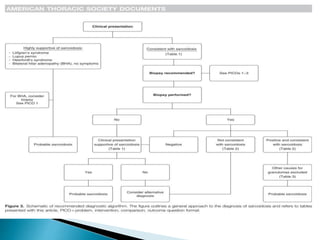
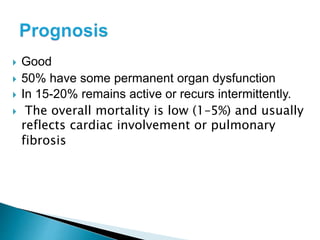
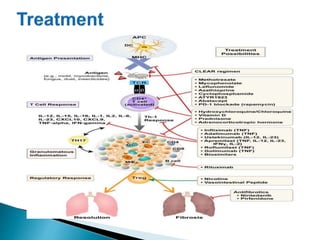
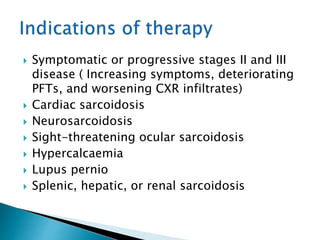
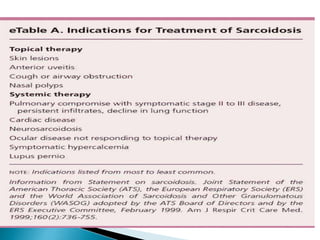
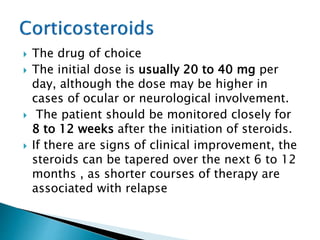
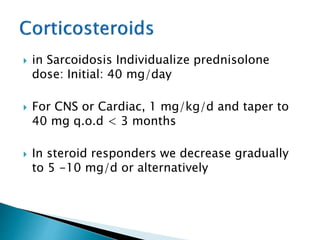
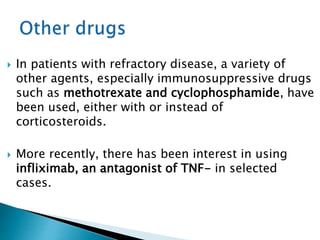
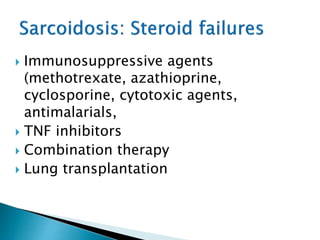
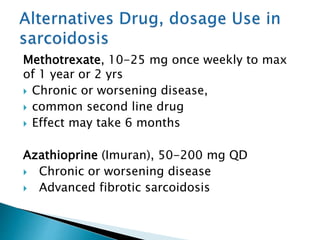
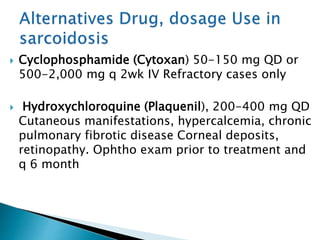
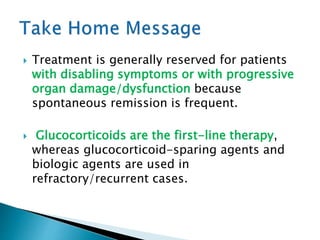
This document provides information on sarcoidosis, a chronic inflammatory disease of unknown cause that most commonly affects the lungs. It discusses the typical presentation and involvement of organs, diagnostic testing including imaging and biopsy findings, differential diagnoses, prognosis, and treatment approaches including corticosteroids as first-line therapy and immunosuppressants for refractory disease. The goal of treatment is to control inflammation and symptoms, with corticosteroids being the mainstay but other agents used if there is no response or for life-threatening disease.