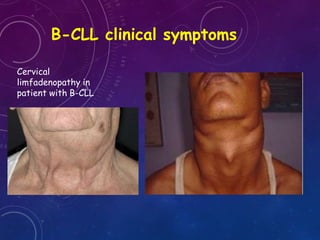
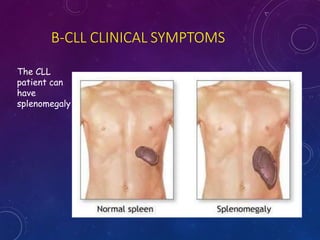
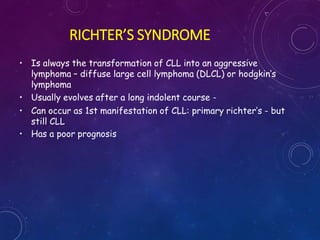
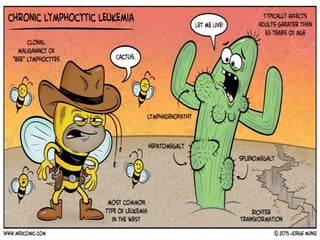
The document discusses chronic lymphocytic leukemia (CLL), including its definition, epidemiology, etiology, pathogenesis, clinical symptoms, diagnosis, staging, prognosis, and treatment. Some key points:
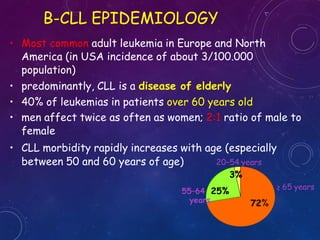
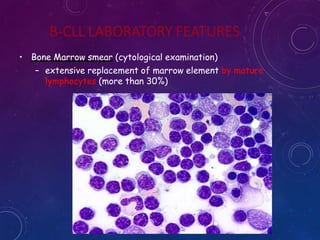
- CLL is characterized by the proliferation and accumulation of small, mature lymphocytes in the blood, bone marrow, and lymphoid tissues. It most commonly affects elderly adults.
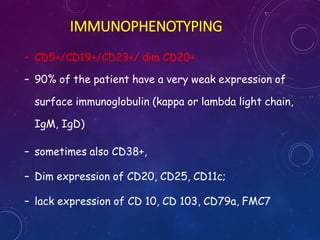
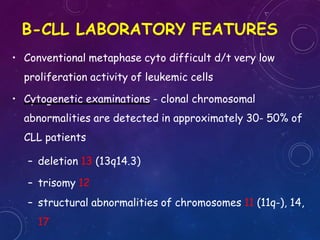
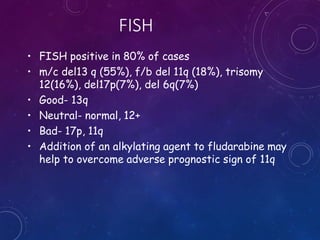
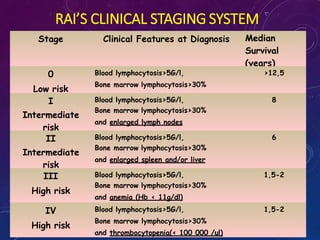
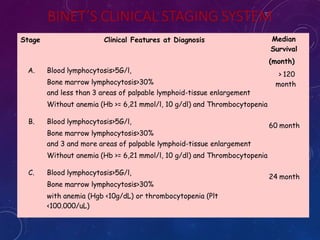
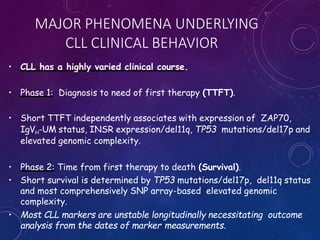
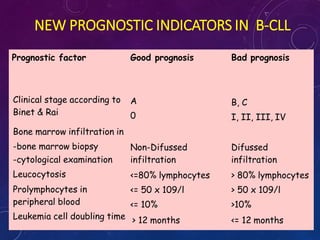
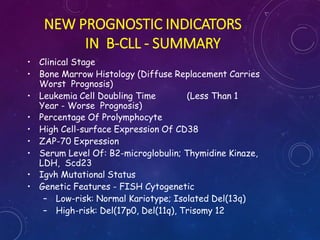
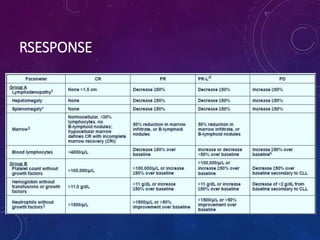
- Diagnosis is based on blood cell counts and immunophenotyping of lymphocytes. Prognosis depends on factors like clinical stage, genomic abnormalities, and biomarker expression levels.
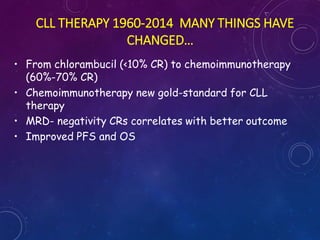
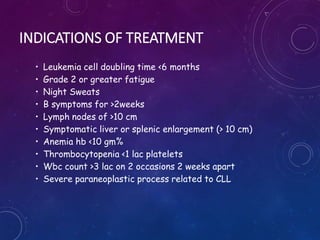
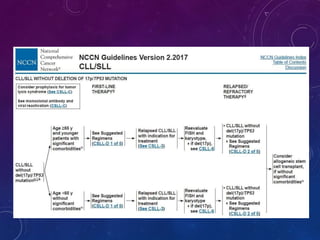
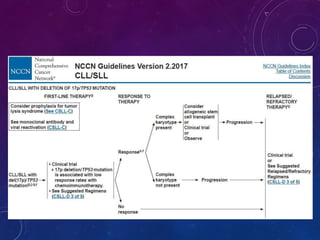
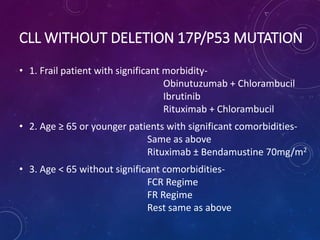
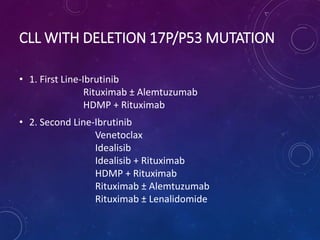
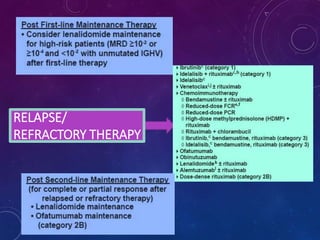
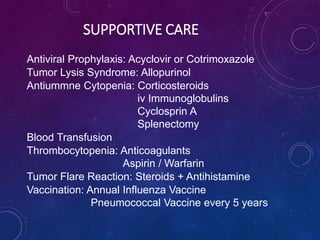
- Treatment involves chemotherapy, chemoimmunotherapy, targeted therapies, and supportive care. The appropriate treatment approach depends on a patient's risk