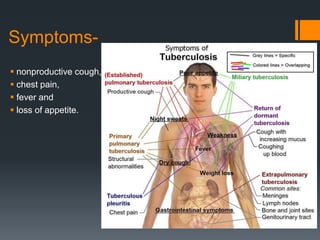
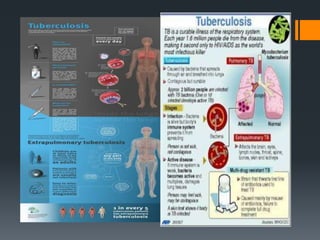
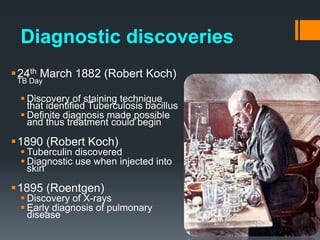
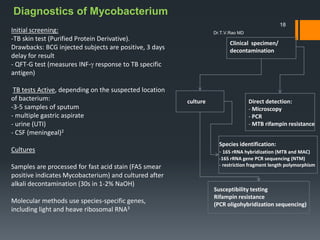
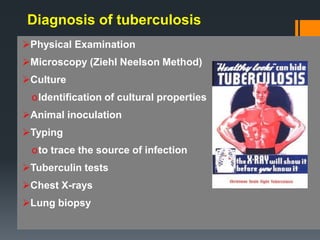
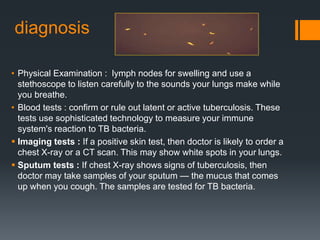
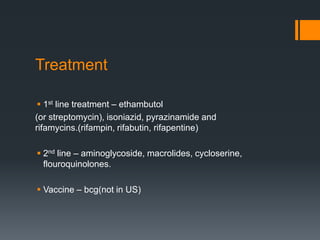
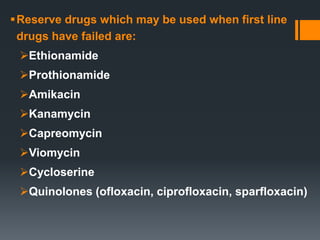
Tuberculosis is a chronic infectious disease caused by the bacterium Mycobacterium tuberculosis. It typically affects the lungs but can affect any part of the body. Risk factors include poverty, crowding, illnesses that weaken the immune system like HIV, and malnutrition. There are two main types - primary tuberculosis occurs in those never exposed before while secondary tuberculosis occurs from reactivation of a previous infection. Diagnosis involves physical exam, sputum tests, chest x-rays, and culture of bacteria. Treatment requires a combination of antibiotics taken for several months. Preventive measures include isolation during early treatment, ventilation, cough hygiene, and masks.