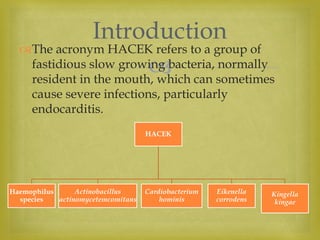
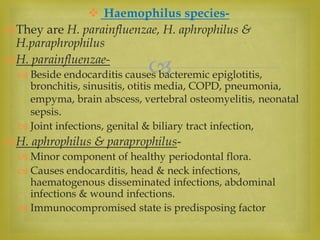
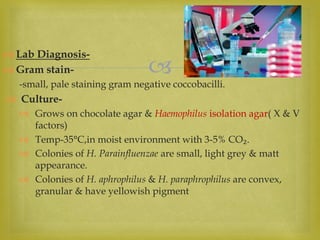
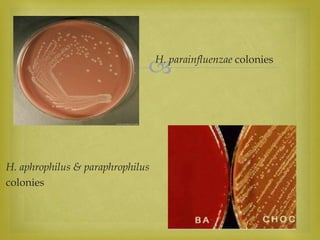
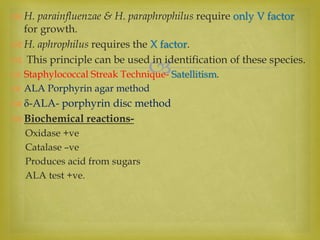
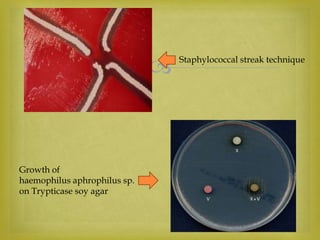
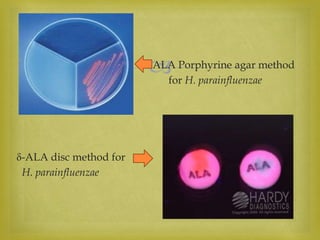
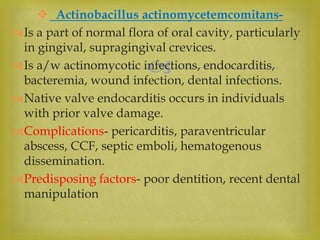
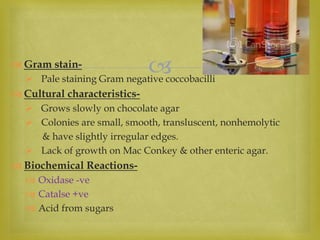
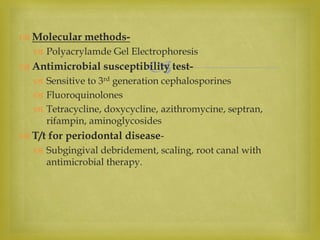
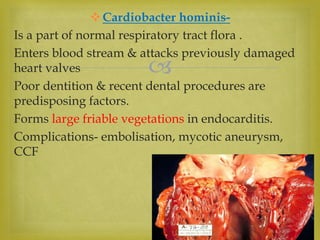
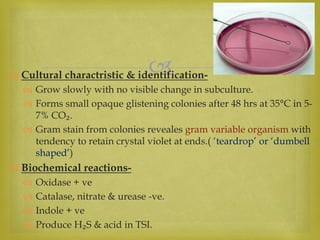
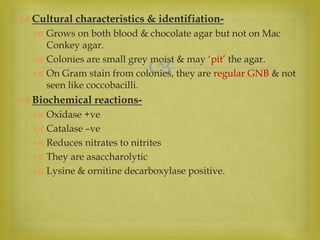
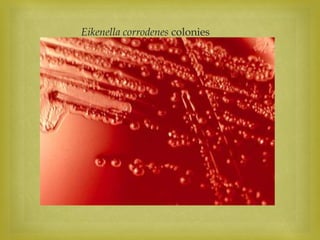
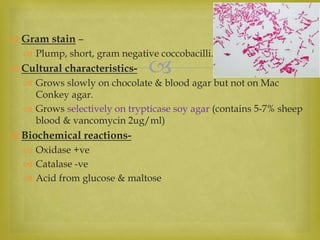
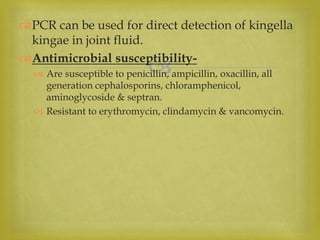
The document summarizes the HACEK group of bacteria - Haemophilus species, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae. It describes their roles as normal flora that can sometimes cause infections like endocarditis. It covers their laboratory identification through gram stains, culture characteristics, and biochemical reactions. It also discusses their antimicrobial susceptibility and treatment considerations.