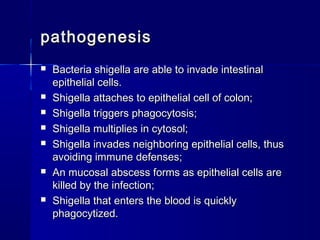
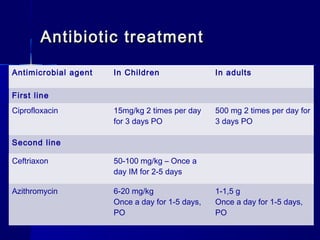
Shigellosis is an intestinal infection caused by Shigella bacteria, leading to severe abdominal cramps, bloody diarrhea, and potential fever. The disease primarily affects young children and is transmitted through fecal-oral routes, often in situations with poor sanitation. Treatment involves antibiotics, rehydration, and management of complications, with isolation of the pathogen from fecal material being the diagnostic gold standard.