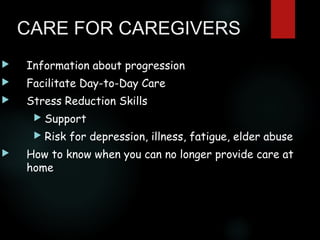
Dementia is a degenerative condition that causes loss of brain function including memory, thinking, language, judgment and behavior. It is caused by damage to the brain that cannot be treated or stopped. There are several types of dementia, with Alzheimer's disease being the most common. Diagnosis is based on memory loss and one or more cognitive impairments. Current therapy focuses on cholinesterase inhibitors to slow progression and stabilize symptoms. Care for dementia patients focuses on establishing routines, minimizing distractions and lowering standards to reduce confusion, agitation and promote independence. Caregiver support and education is important as dementia is stressful and impacts daily life.