Dr. D. SUVANKAR discusses anesthesia considerations for various ENT endoscopic procedures including bronchoscopy, microlaryngoscopy, and esophagoscopy. Key points include:
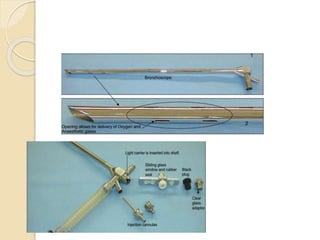
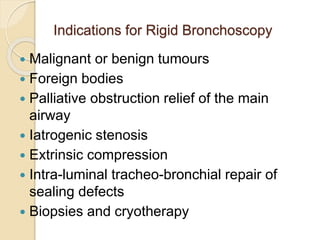
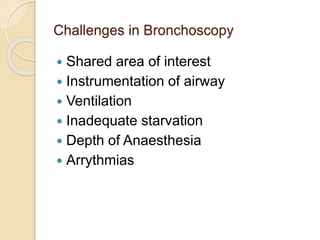
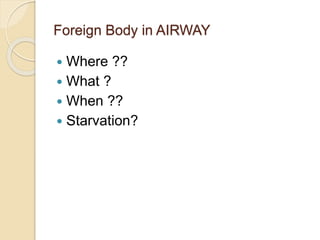
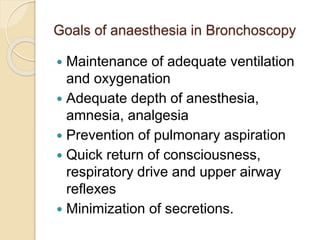
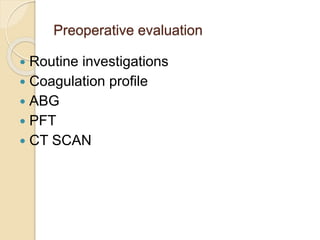
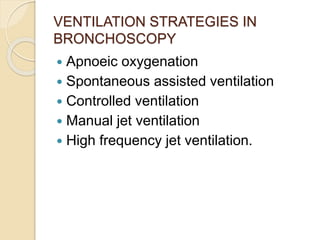
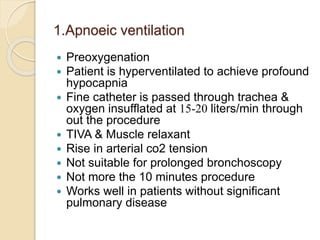
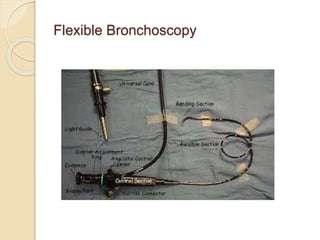
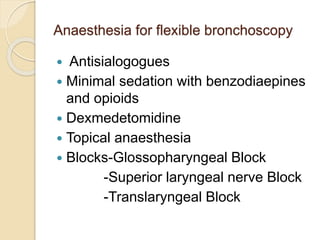
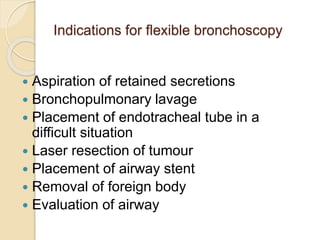
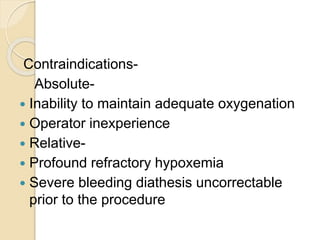
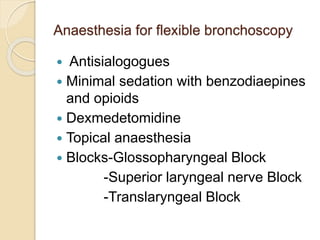
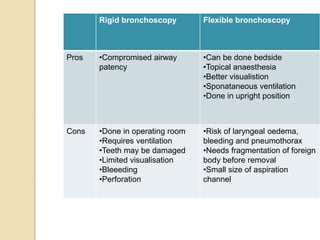
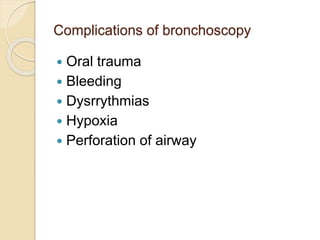
1. Rigid bronchoscopy allows direct visualization of the airway but requires ventilation, while flexible bronchoscopy can be done with minimal sedation.
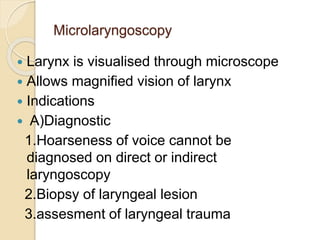
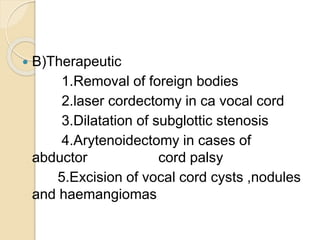
2. Microlaryngoscopy provides magnified visualization of the larynx and allows for precision procedures like laser surgery.
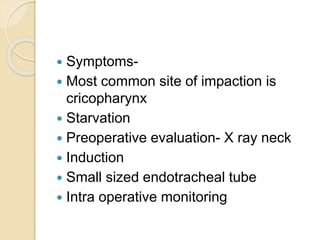
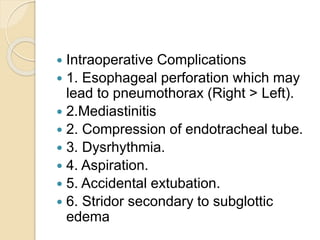
3. Esophagoscopy is commonly used to remove foreign bodies from the esophagus in ENT and requires general anesthesia in children to prevent aspiration if the object dislodges.