1. The document discusses tracheostomy and anaesthesia considerations for microlaryngeal surgery. It covers the definition, history, steps of the procedure, complications, types of tubes, and techniques for airway management including endotracheal intubation and jet ventilation.
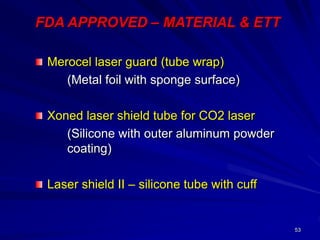
2. Lasers are commonly used in microlaryngeal surgery and ENT procedures. Safety precautions are required due to the risks of burns, fires and smoke inhalation. Special endotracheal tubes coated in metal foil or other fire-resistant materials help protect the airway during laser use.
3. Careful planning is needed for airway management and ventilation during these delicate procedures to provide optimal surgical conditions while protecting the patient's air