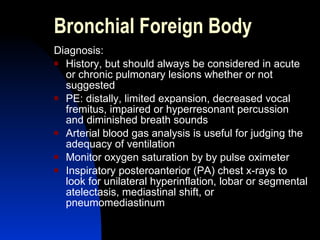
Foreign body aspiration, commonly known as choking, is a serious risk especially for young children. It is a leading cause of accidental death, with nuts and small, round objects posing the biggest hazards. Symptoms depend on the location and size of the object, ranging from mild cough to life-threatening airway obstruction. Diagnosis involves x-rays and bronchoscopy; prompt removal of the object is important to prevent complications like pneumonia. Prevention focuses on careful supervision of young children and avoiding small, hard objects that could be aspirated.