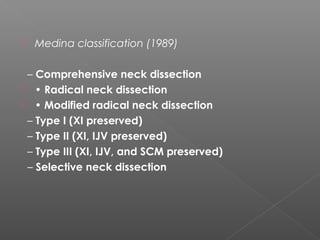
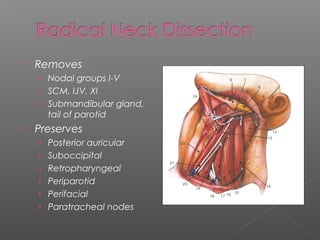
This document discusses the history and anatomy of neck dissections for head and neck cancer. It traces developments from the late 19th century of increasingly conservative neck dissections to preserve important structures. It describes the levels and boundaries of lymph node groups involved in the neck dissection staging system, including levels I-V. Key structures like the hypoglossal nerve and spinal accessory nerve are discussed in relation to the lymph node groups.