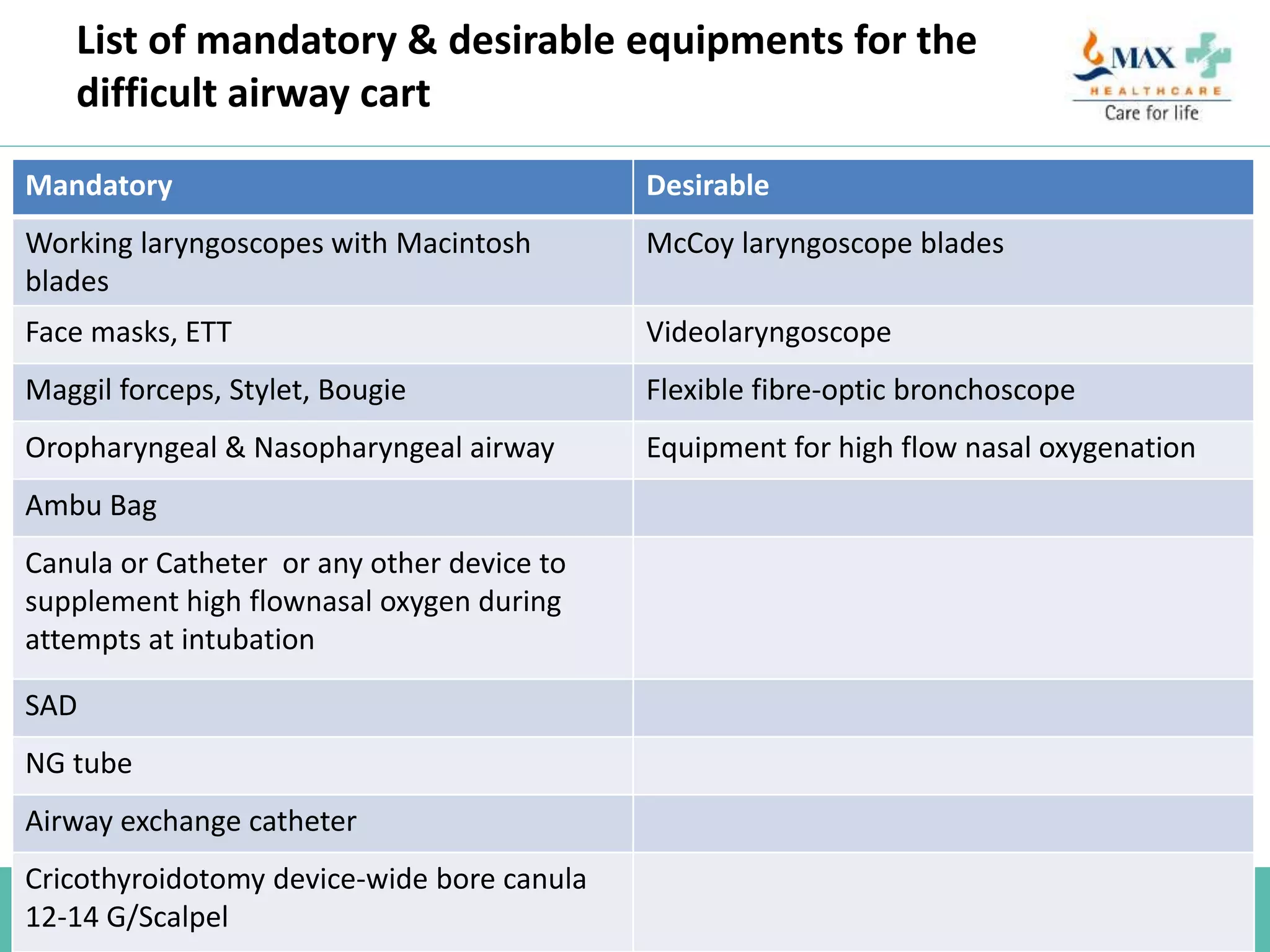
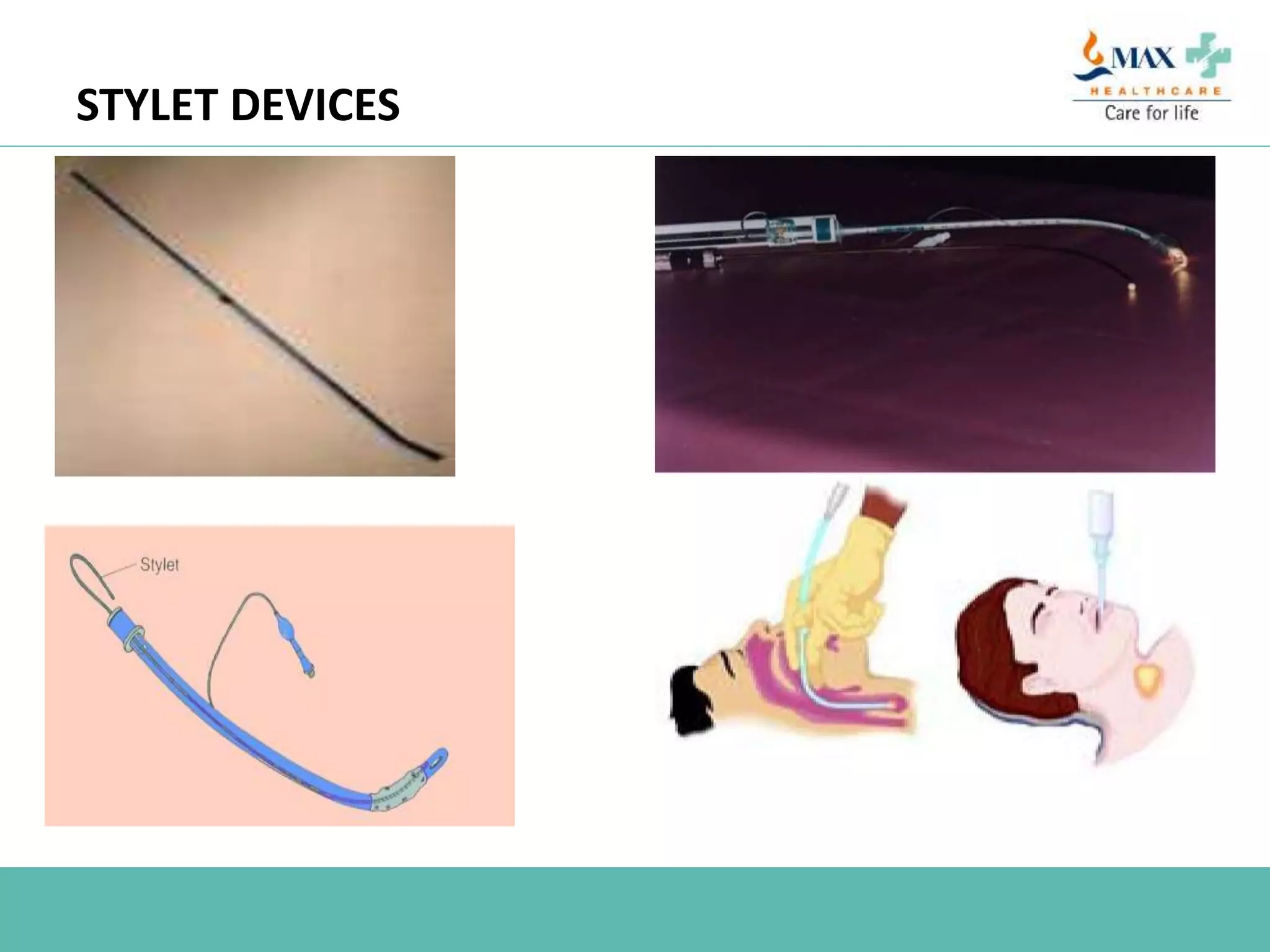
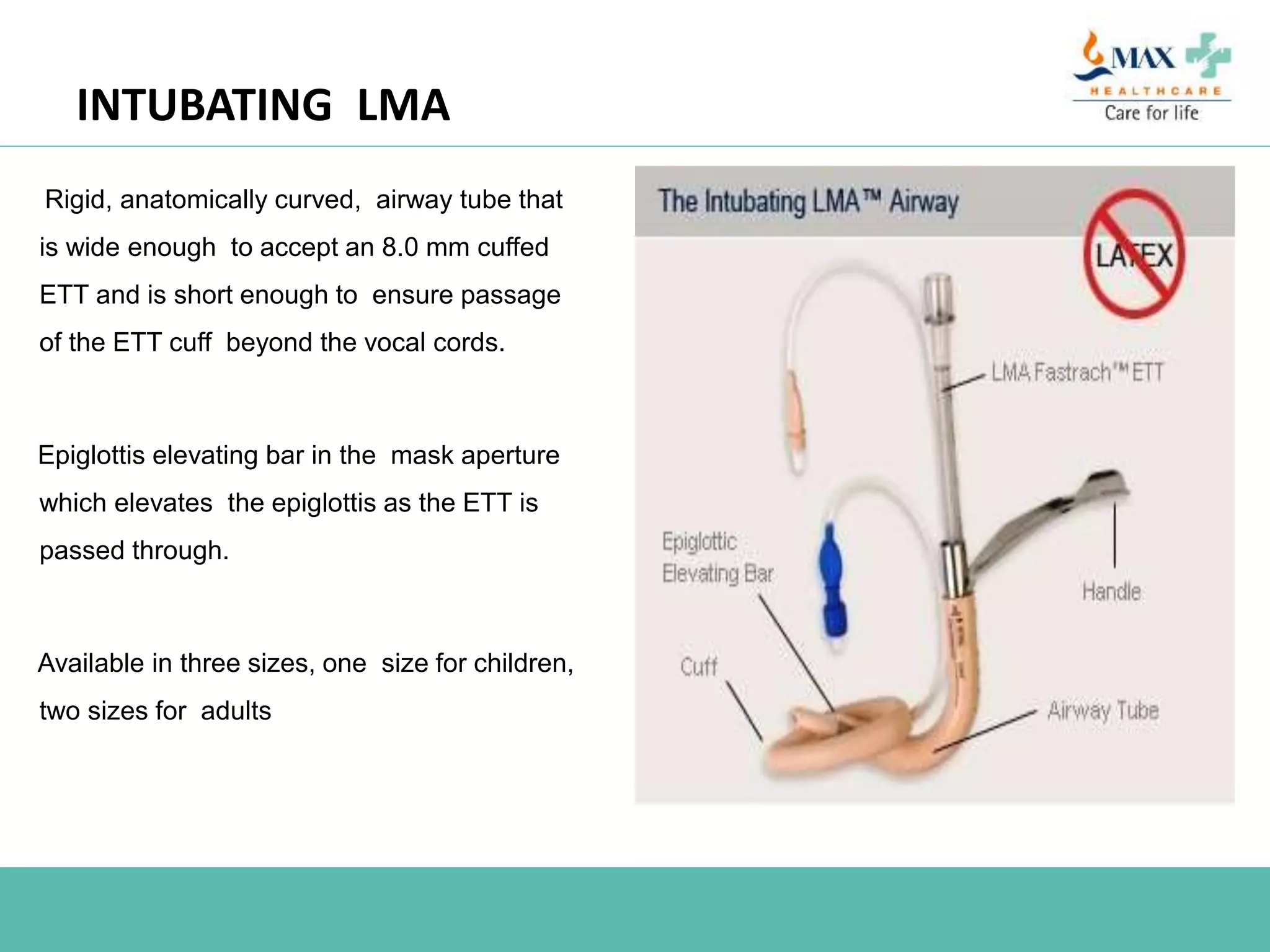
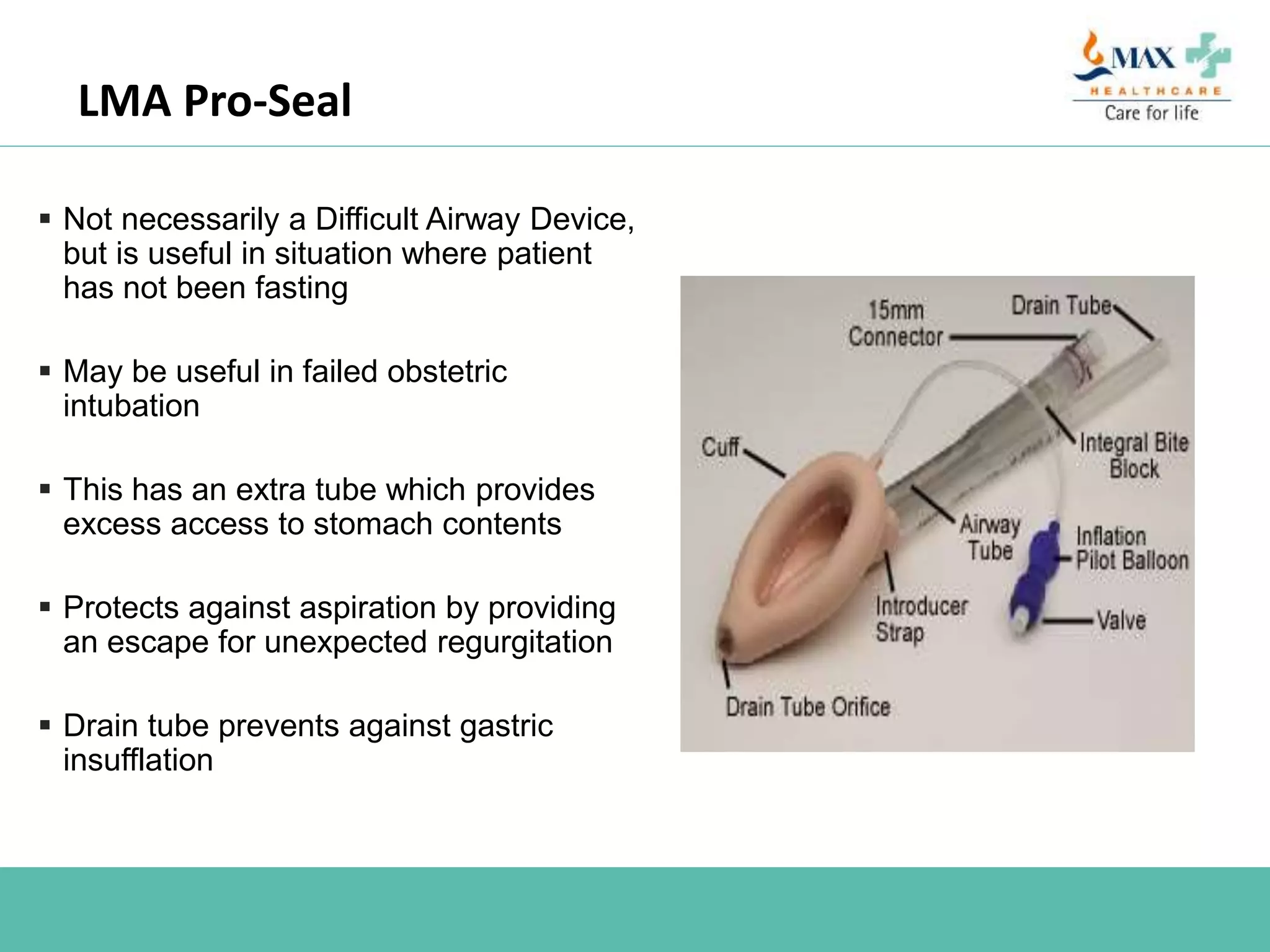
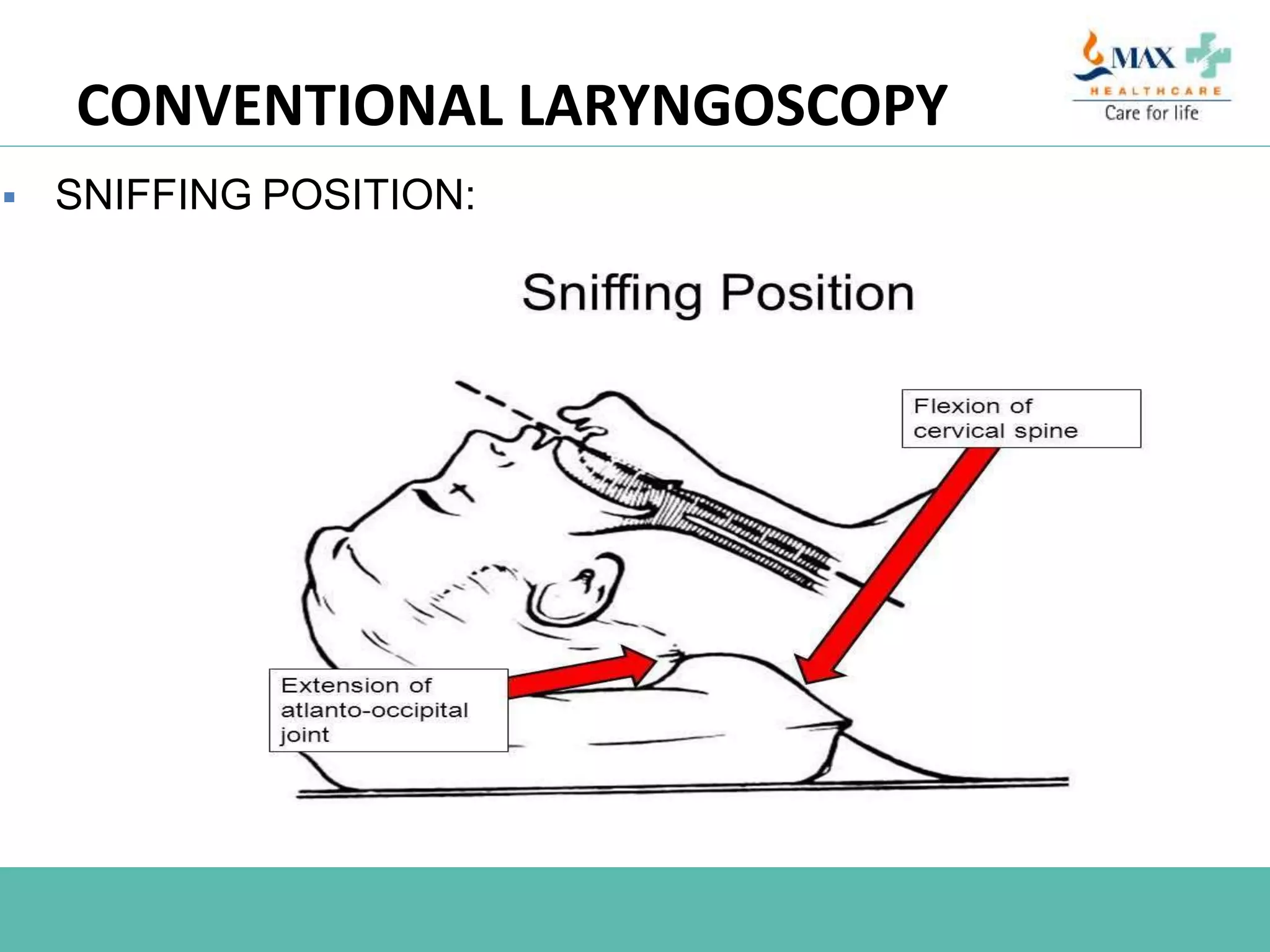
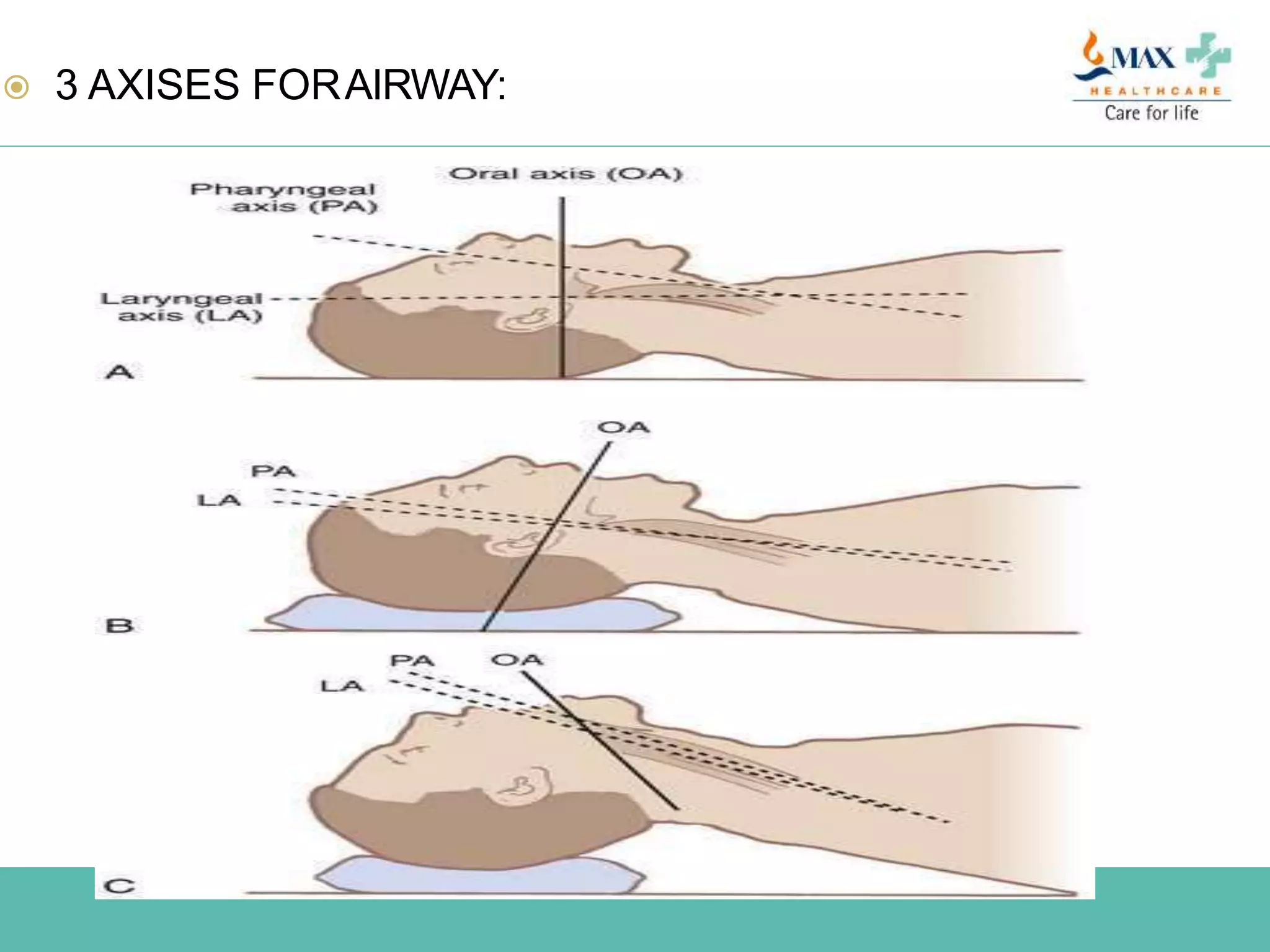
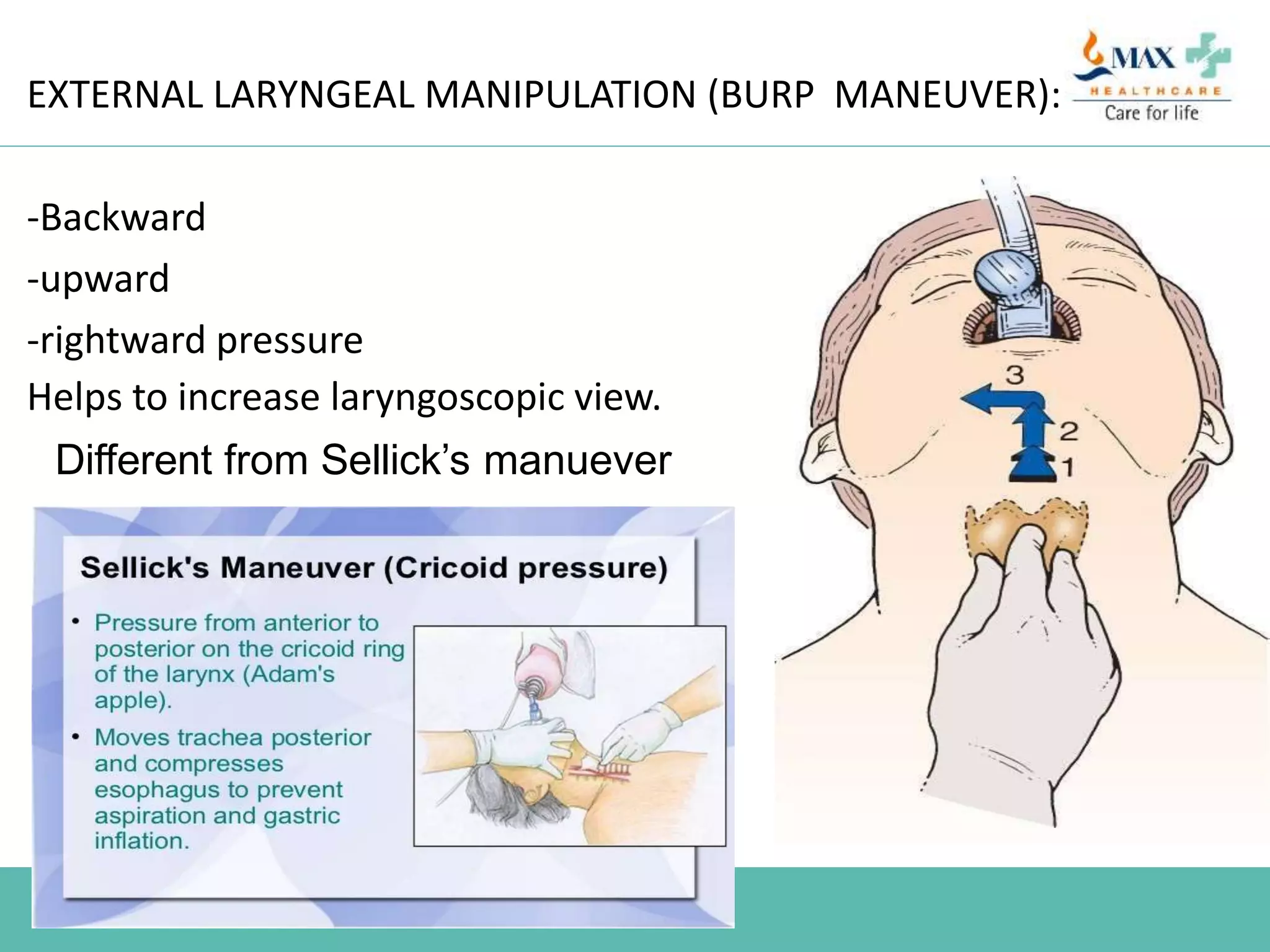
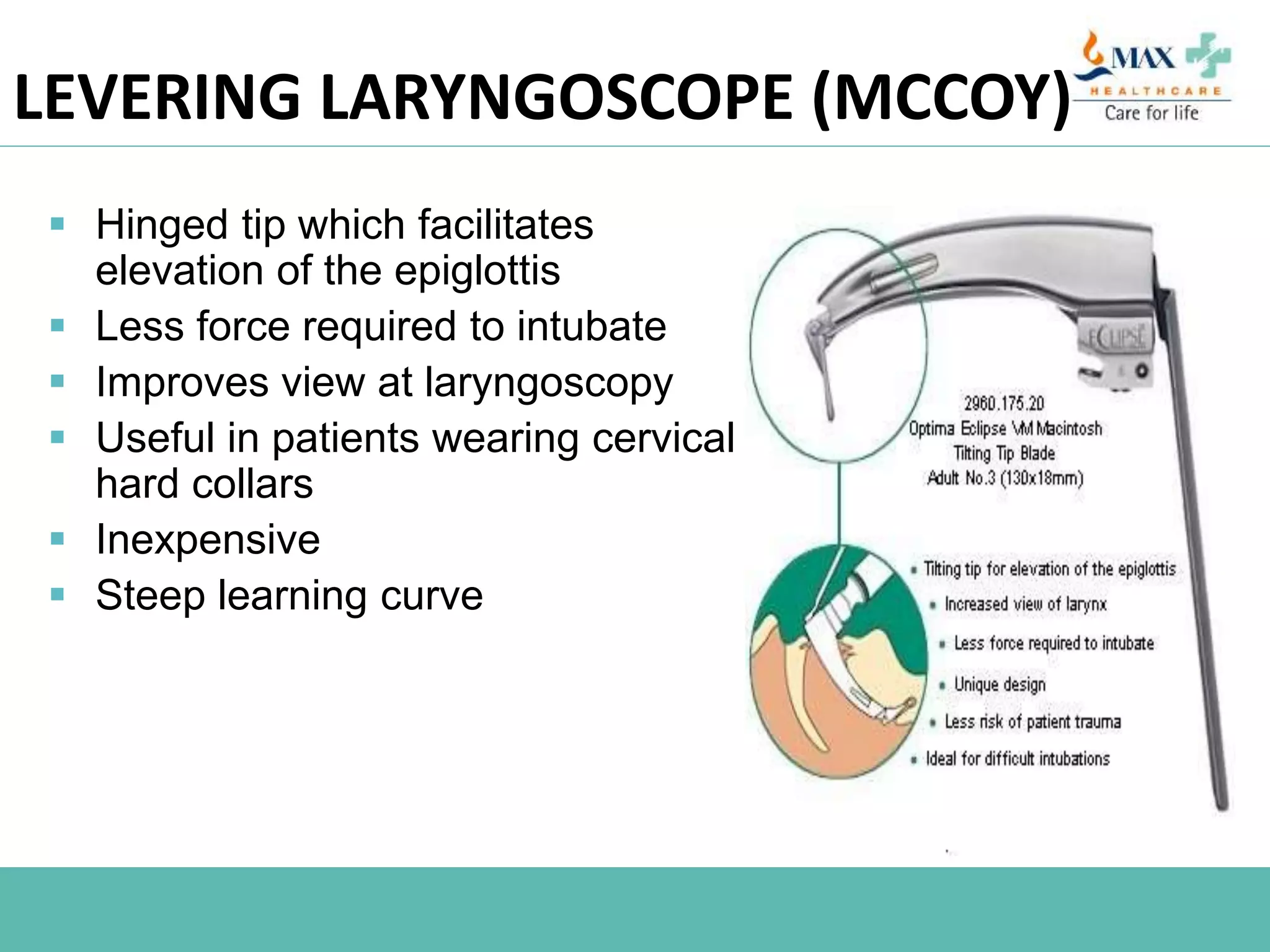
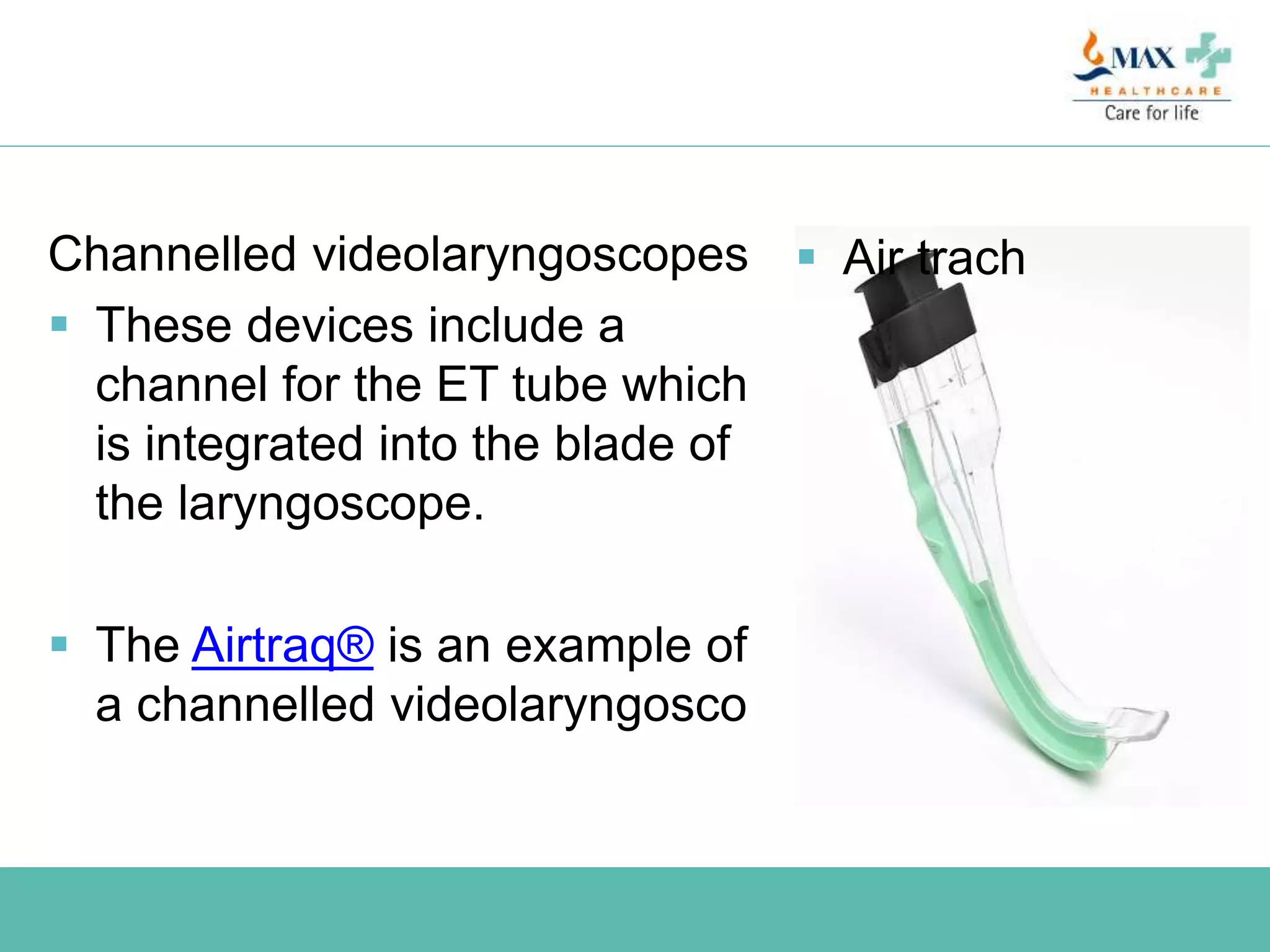
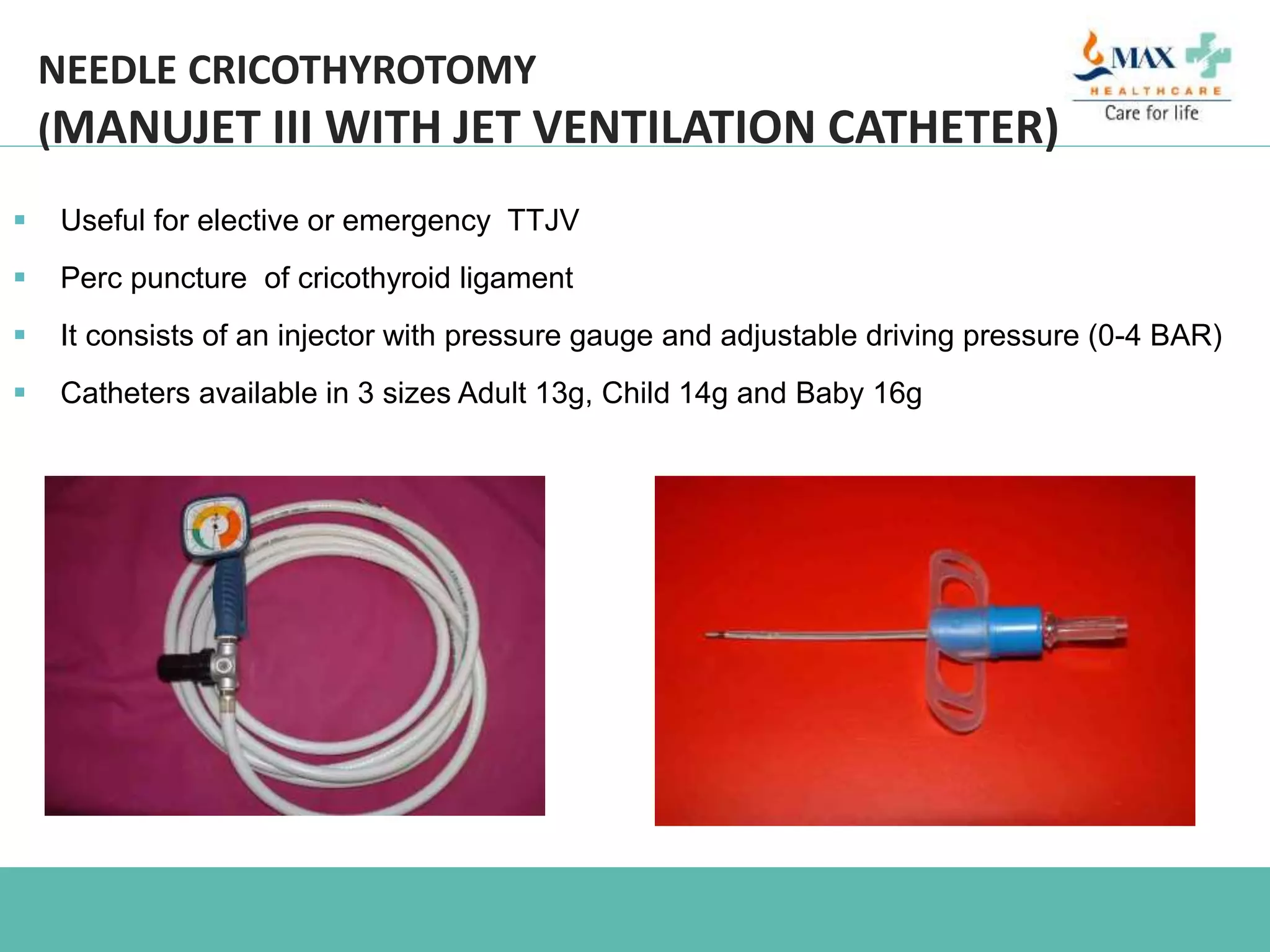
This document provides an overview of difficult airway management in the ICU. It discusses factors that can lead to difficult intubation in ICU patients such as remote location, unstable physiology, and patient factors. It describes different techniques for managing the difficult airway including anticipated difficult airways, unanticipated difficult airways, and cannot intubate/cannot ventilate scenarios. Equipment for difficult airways is outlined including video laryngoscopes, fiberoptic scopes, supraglottic airway devices, and surgical airway options like needle cricothyroidotomy. Pre-oxygenation techniques and adjuncts to improve laryngoscopy views are also summarized.