The document discusses tracheostomy, including its history, definitions, indications, types, procedures, complications, and care. Some key points:
- Tracheostomy can be traced back to 3600 BC in Egypt and was standardized in technique in the 1920s. Modern percutaneous tracheostomy developed in 1969.
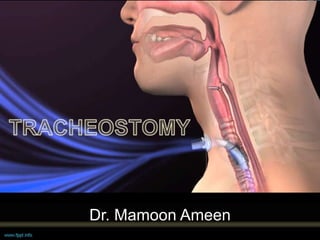
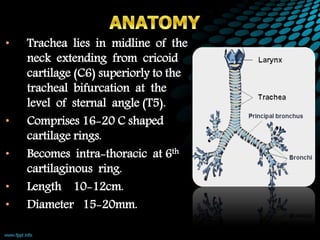
- It involves creating a stoma in the trachea that allows for insertion of a tracheostomy tube to bypass upper airway obstruction and facilitate pulmonary ventilation and toilet.
- Surgical procedures include open tracheostomy and percutaneous tracheostomy. Complications include bleeding, injury to nearby structures, and long term issues like stenosis.
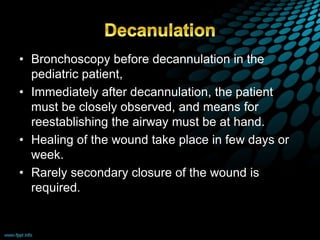
- Ongoing care involves tube maintenance,