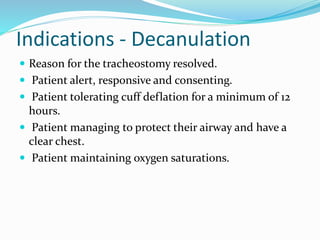
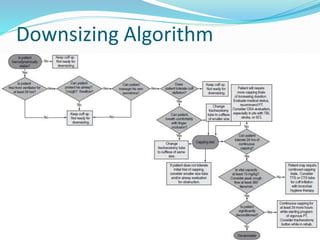
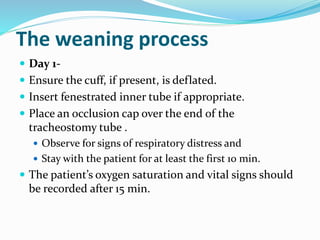
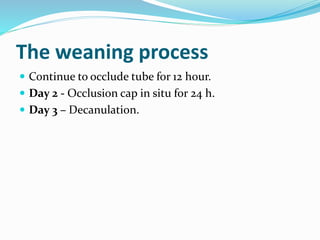
The document outlines protocols for tracheostomy care and decannulation, detailing hygiene, cuff pressure management, tube changes, and patient assessment needed to safely transition patients. It emphasizes the multi-disciplinary team's roles, including ENT surgeons and therapists, in evaluating and preparing patients for decannulation, focusing on systematic approaches to ensure patient safety. Key indicators for decannulation include patient's awareness, airway protection, cuff deflation tolerance, and maintaining adequate oxygen saturation.