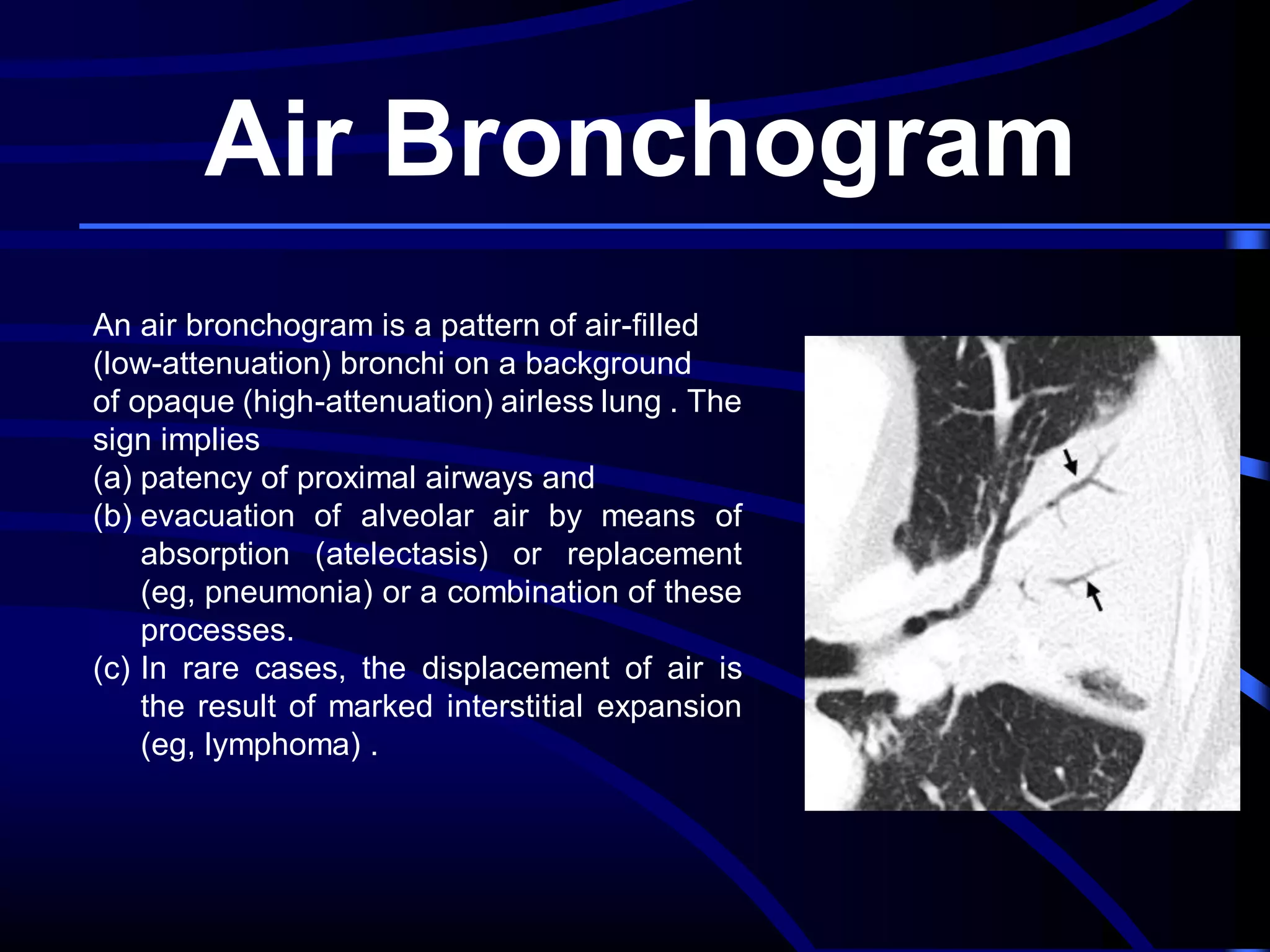
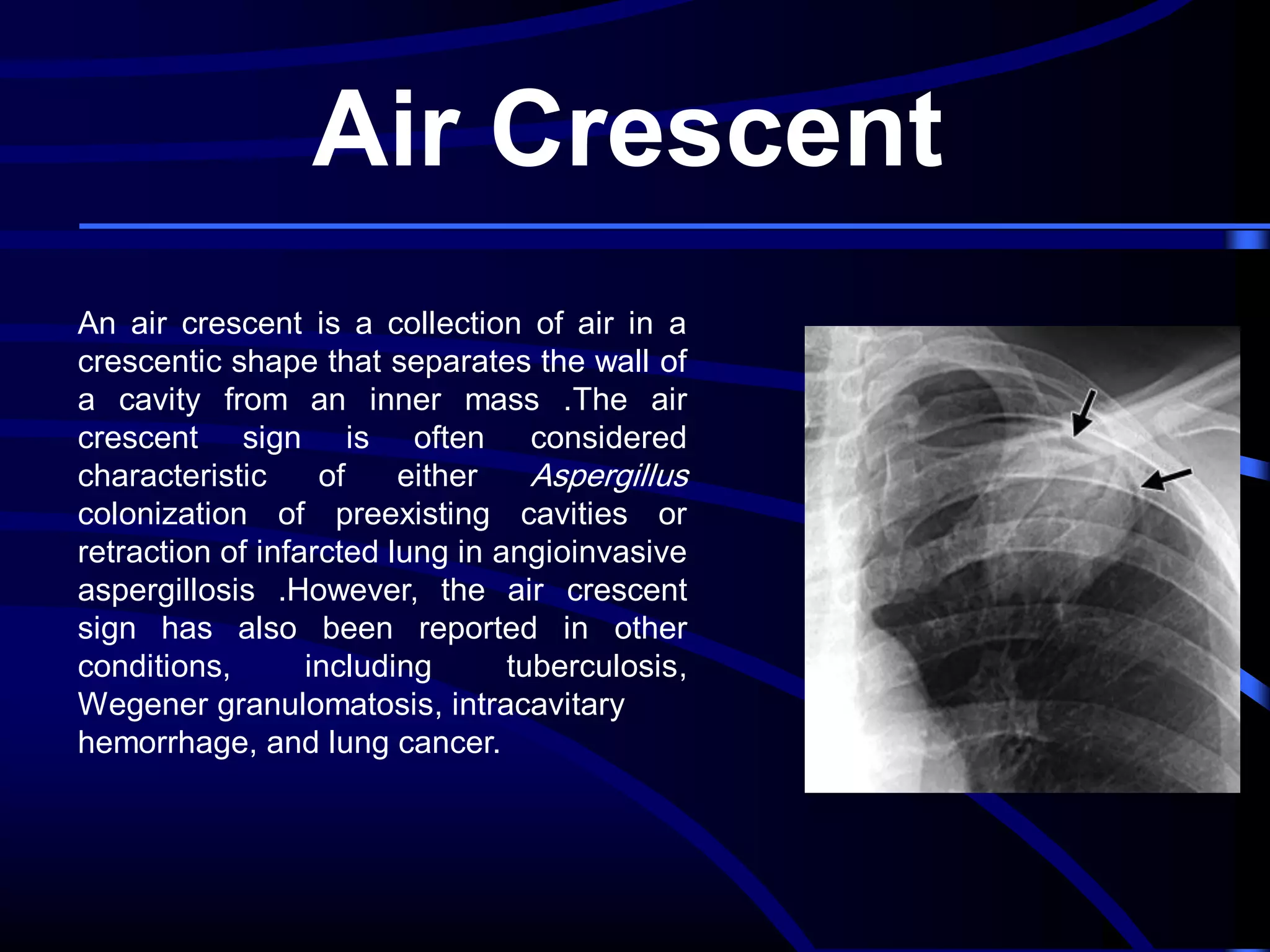
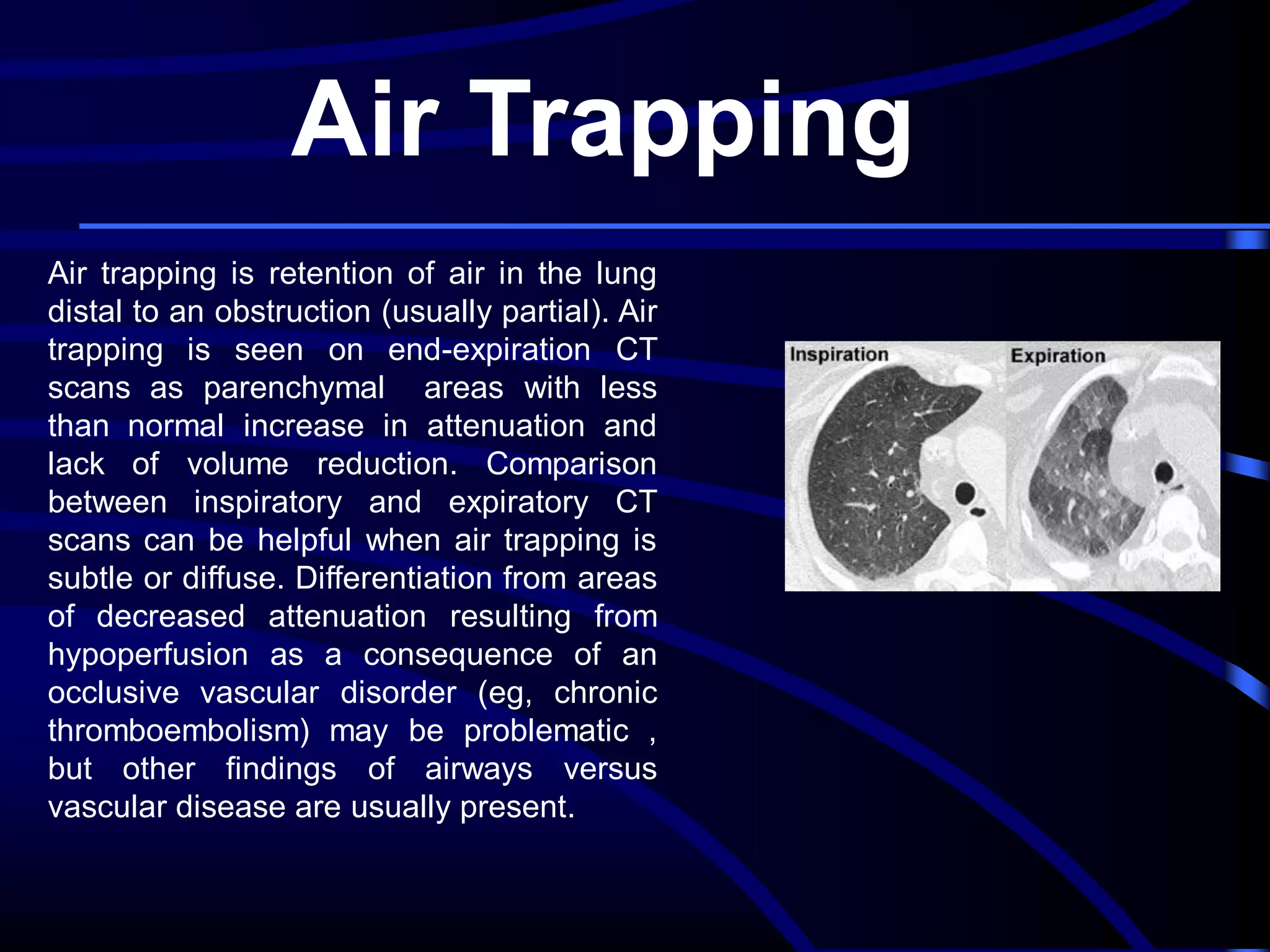
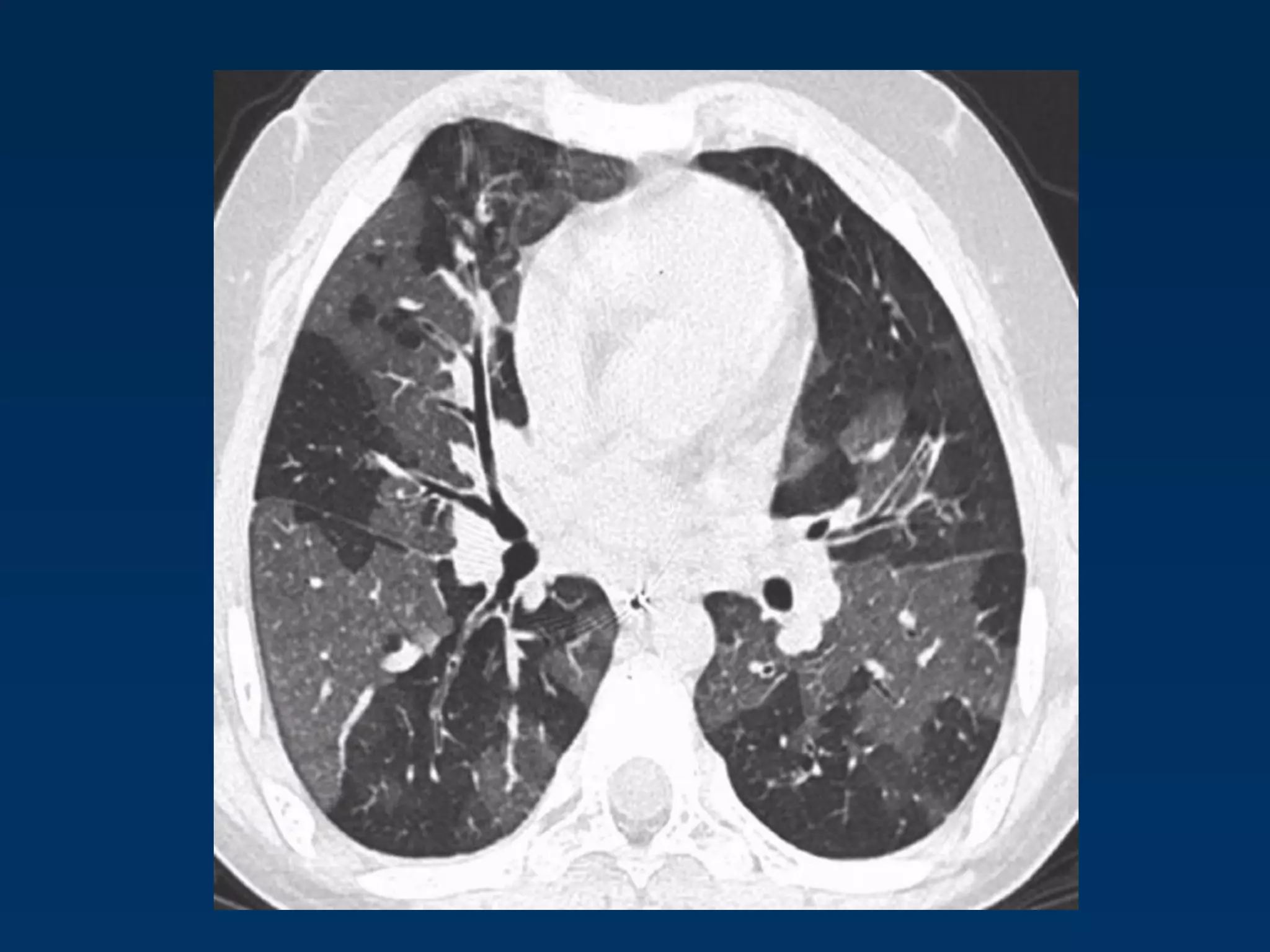
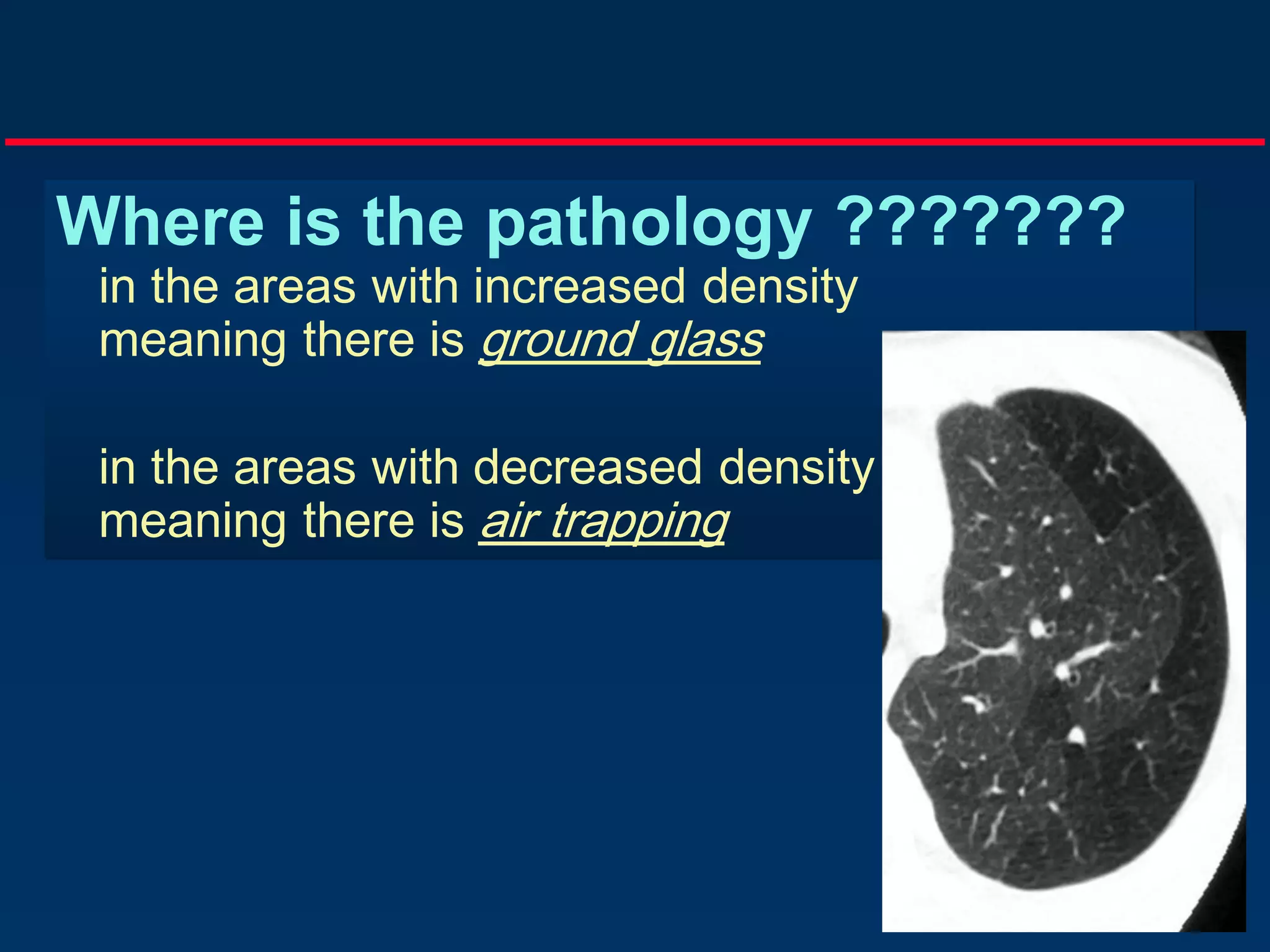
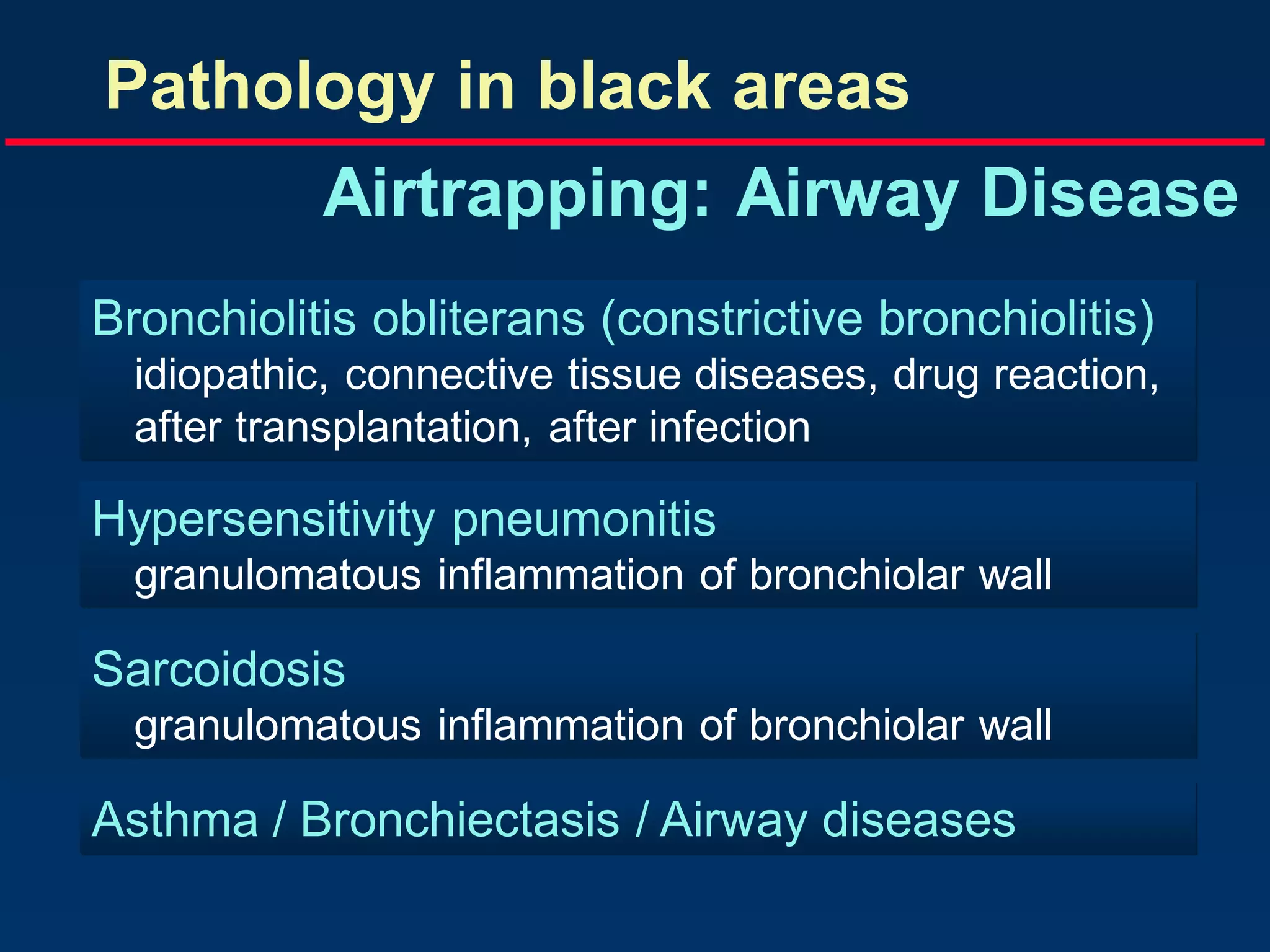
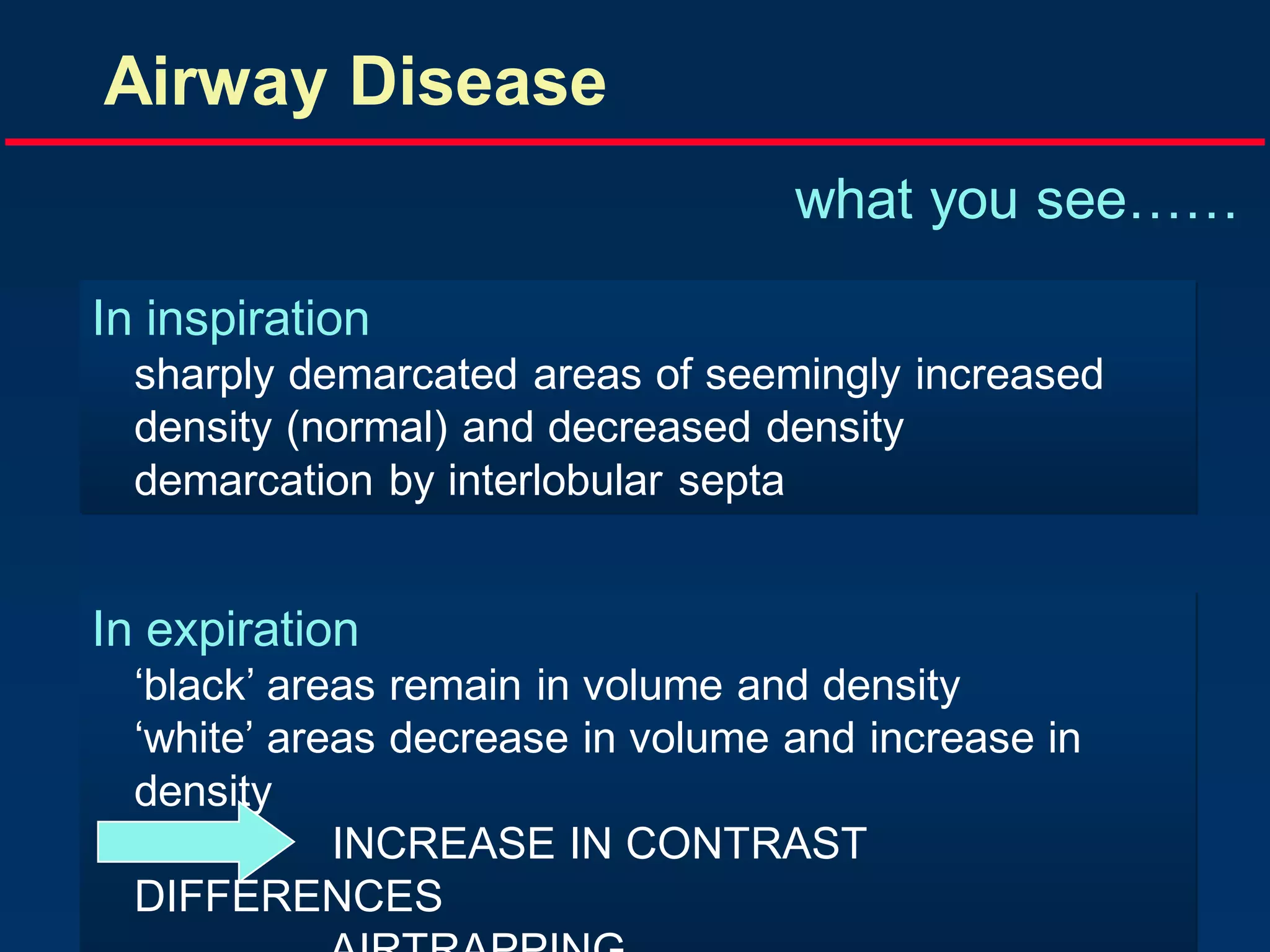
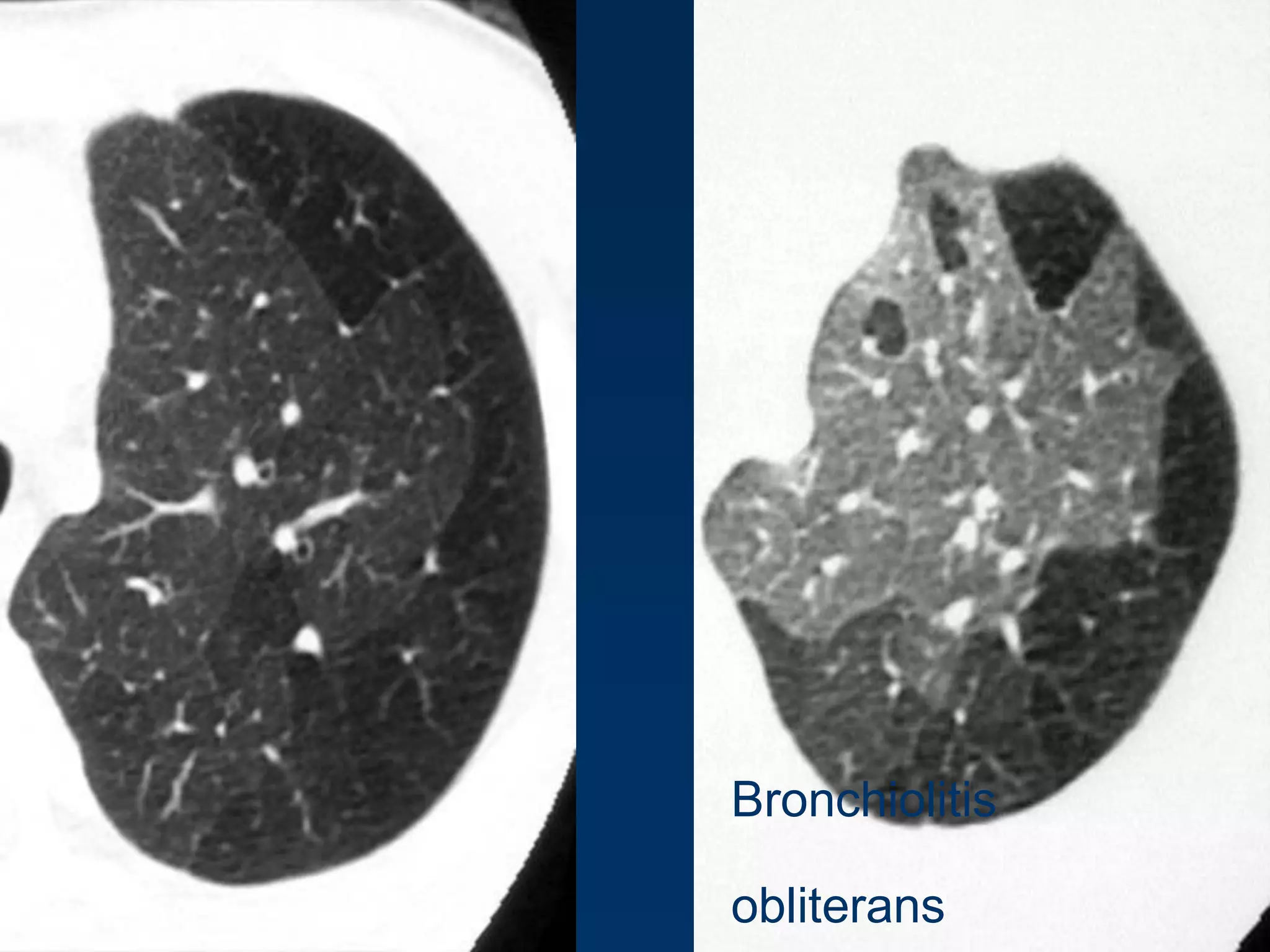
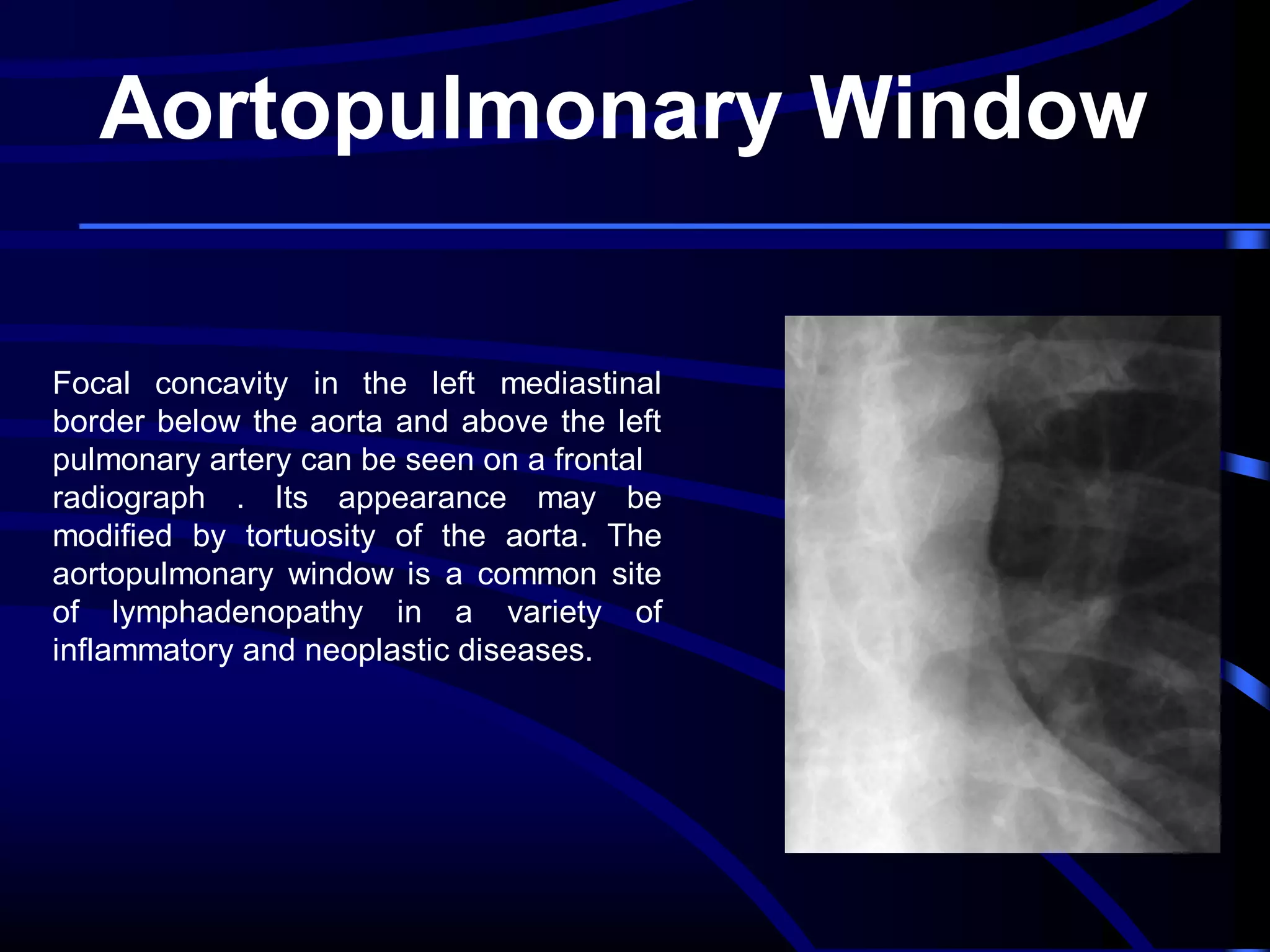
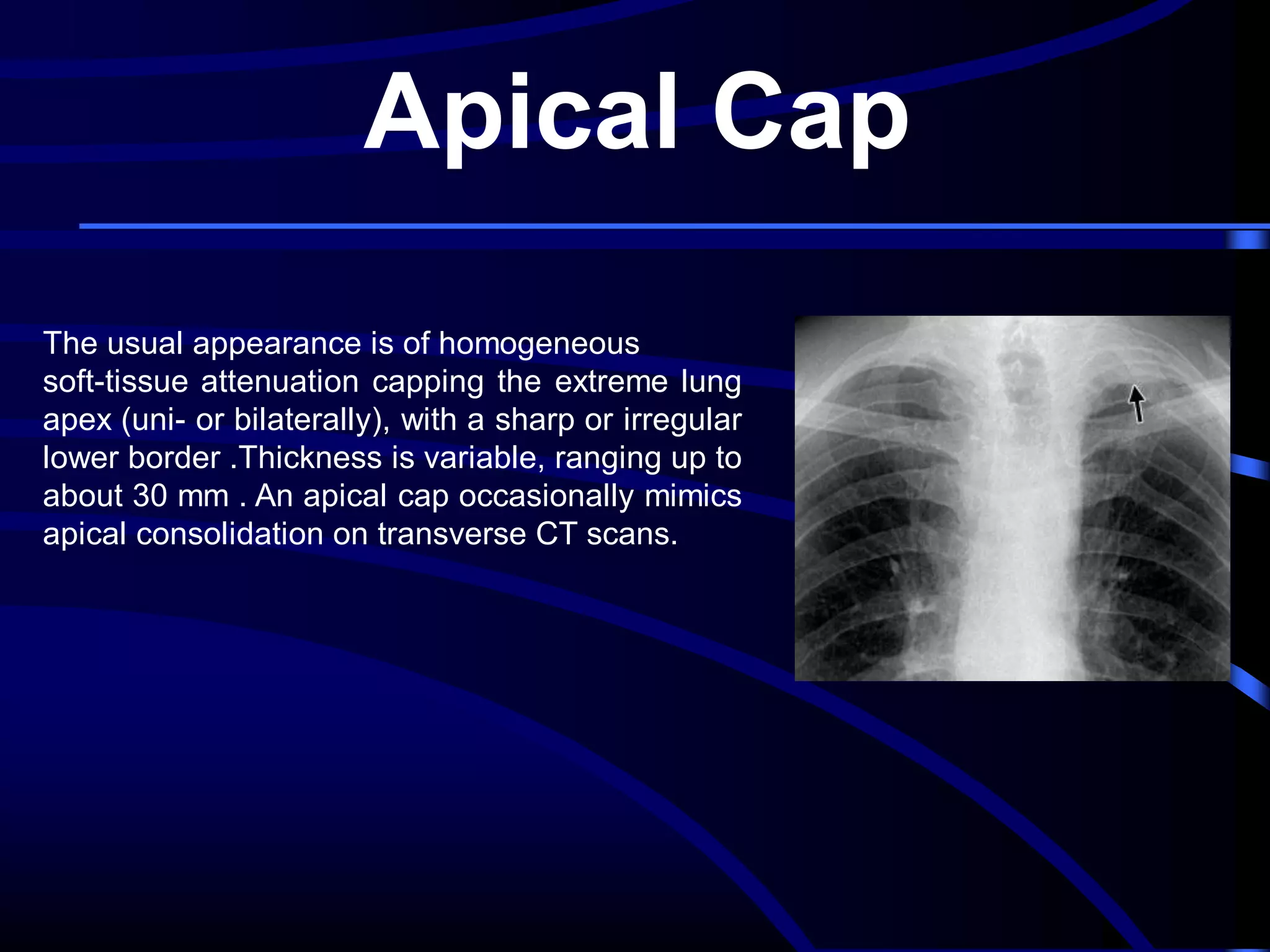
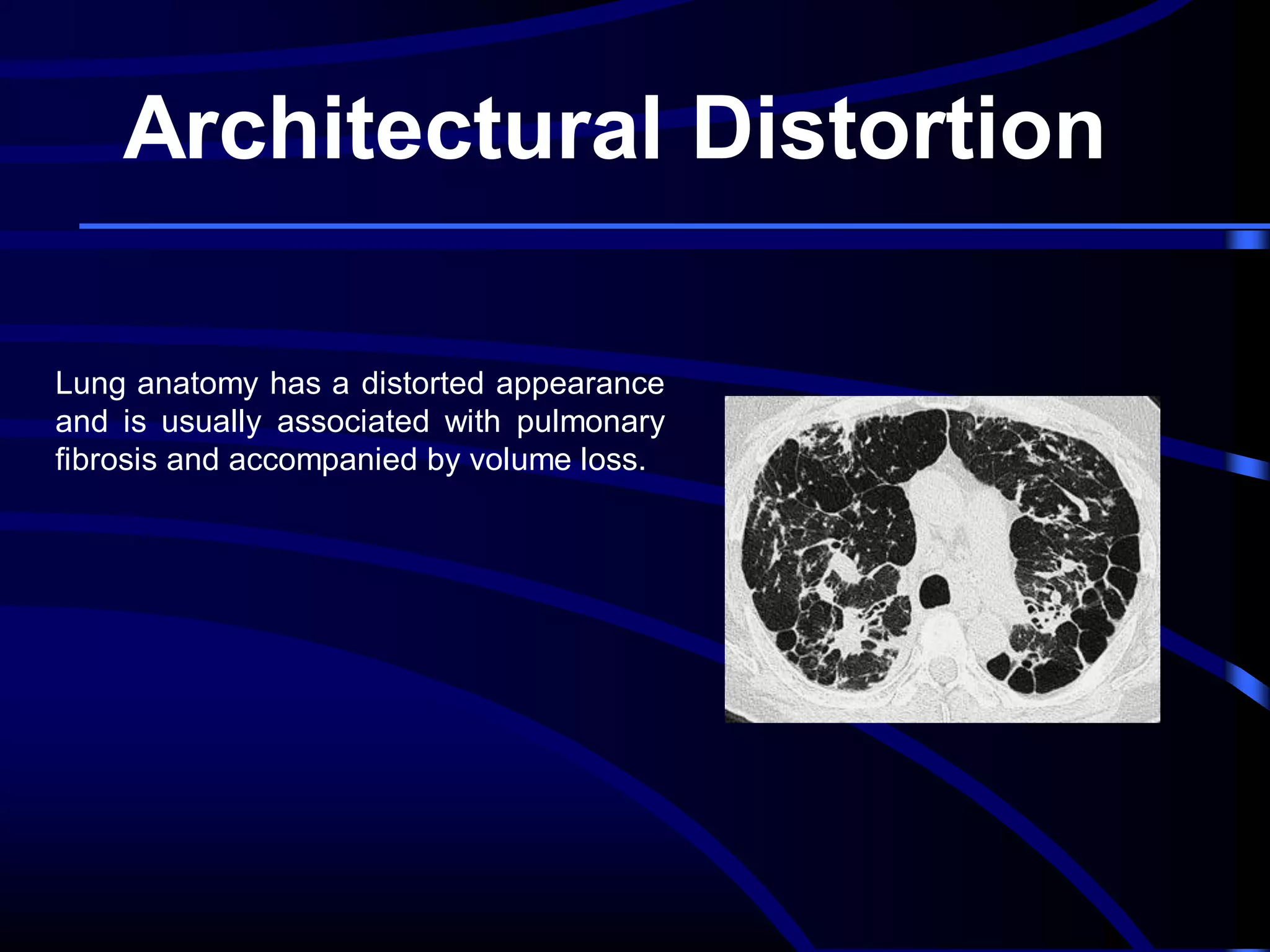
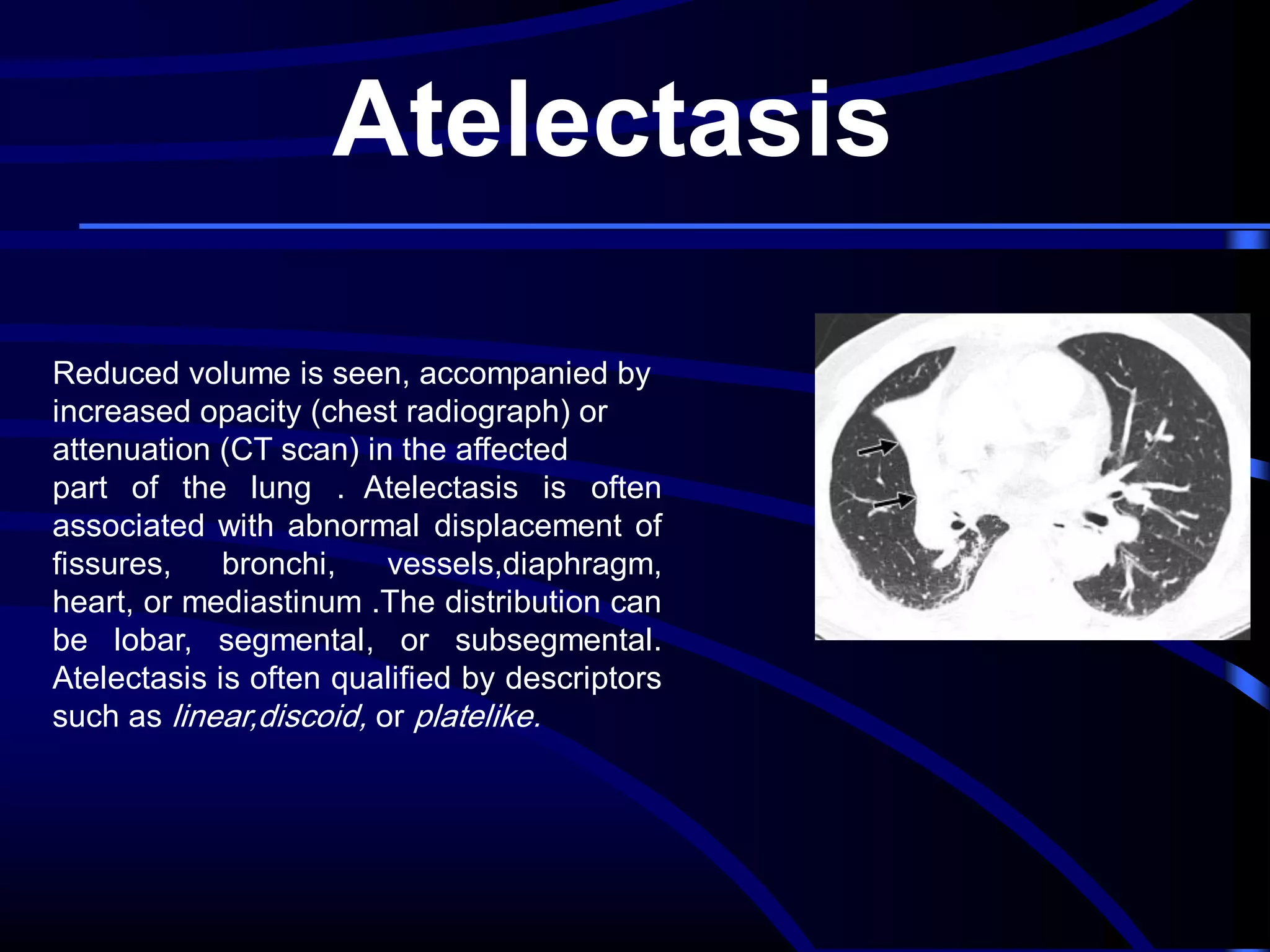
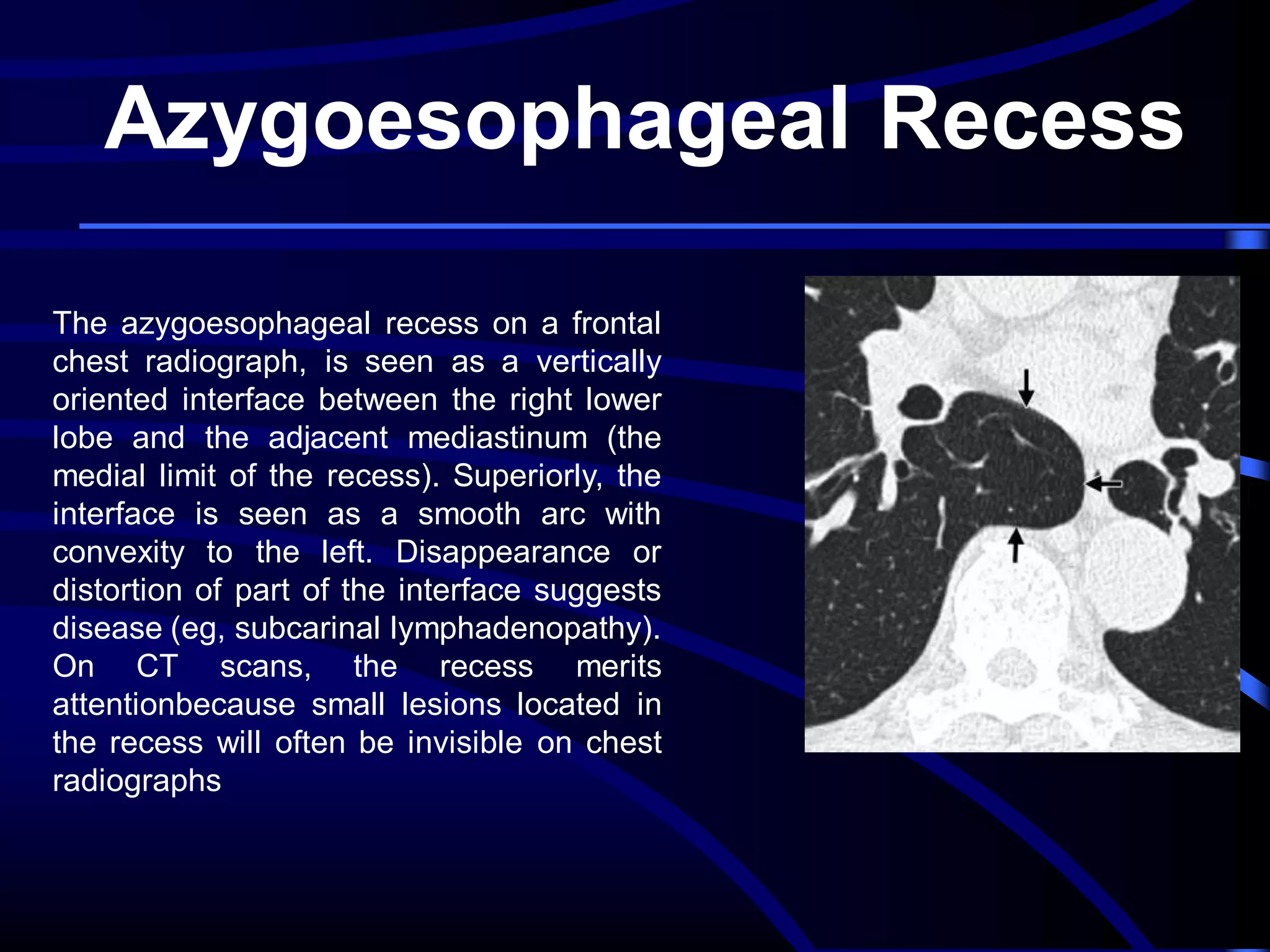
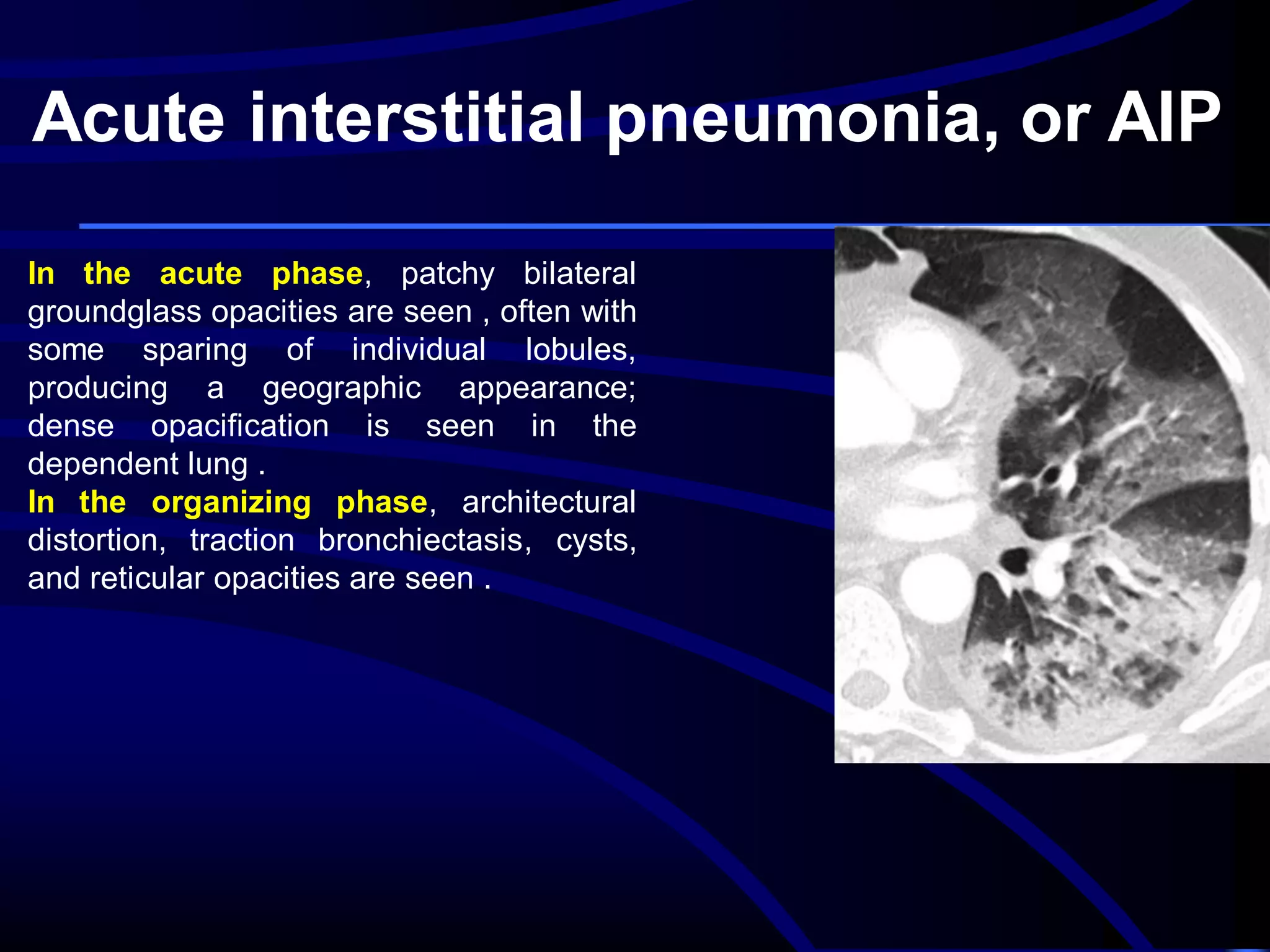
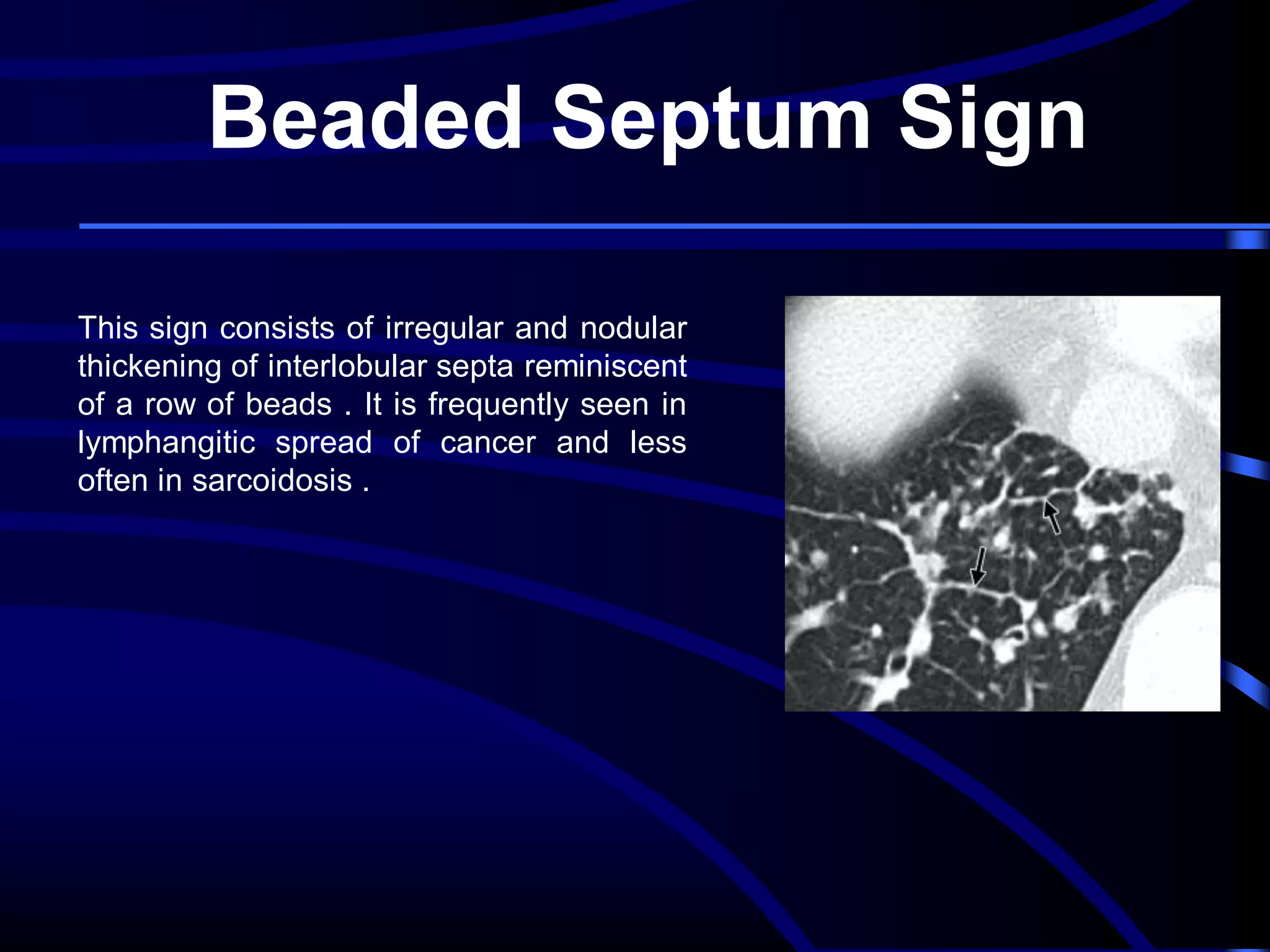
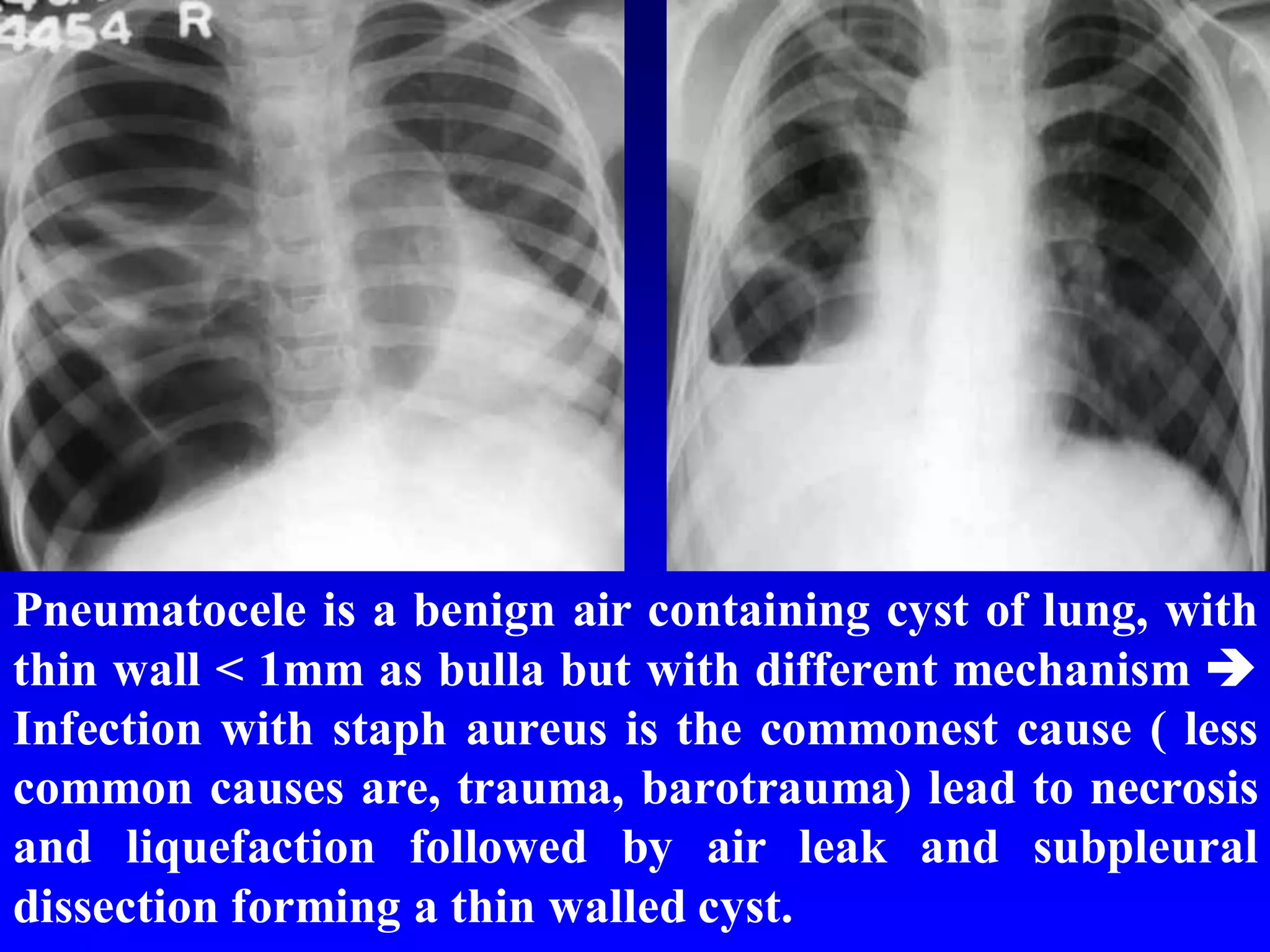
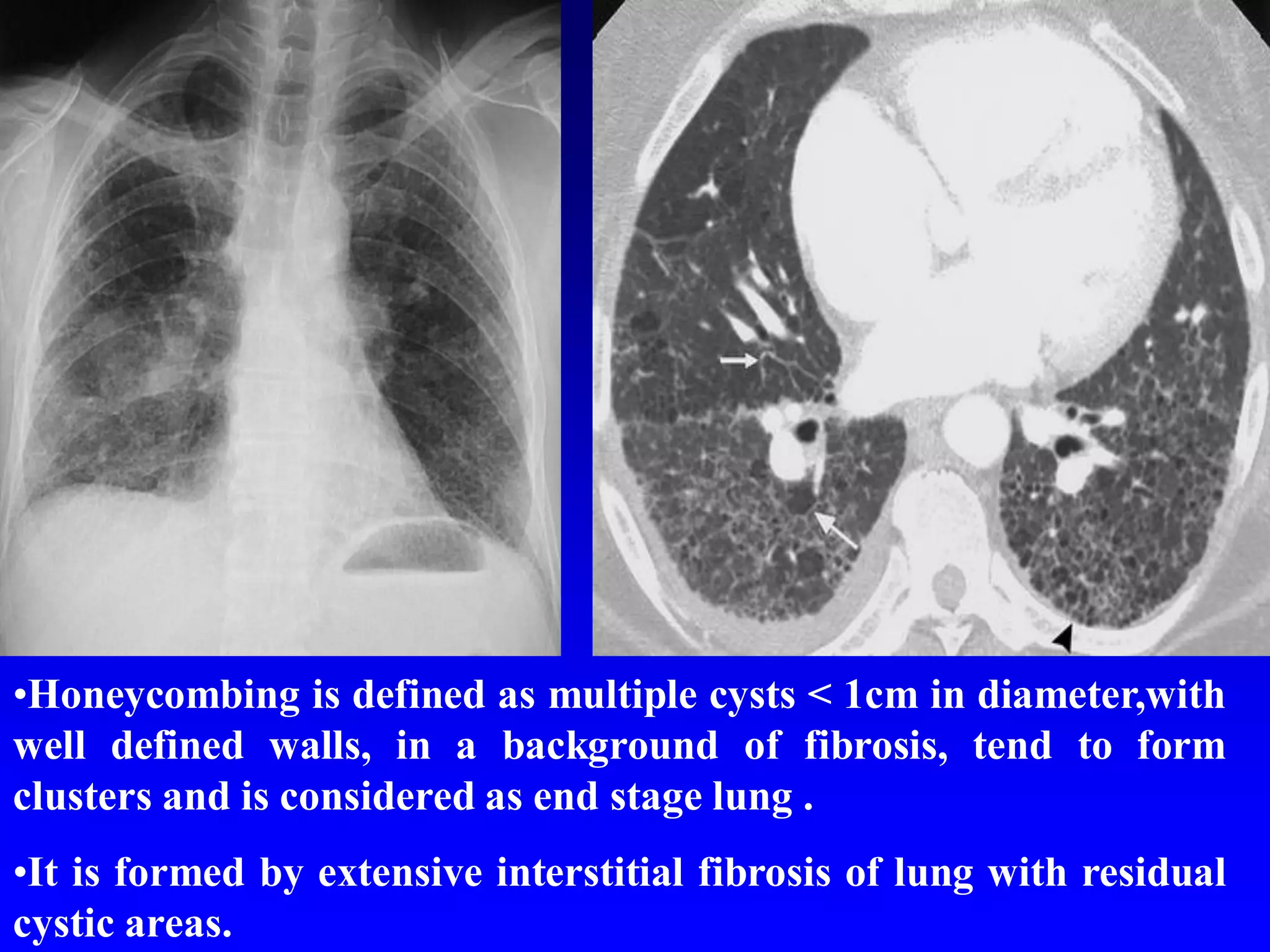
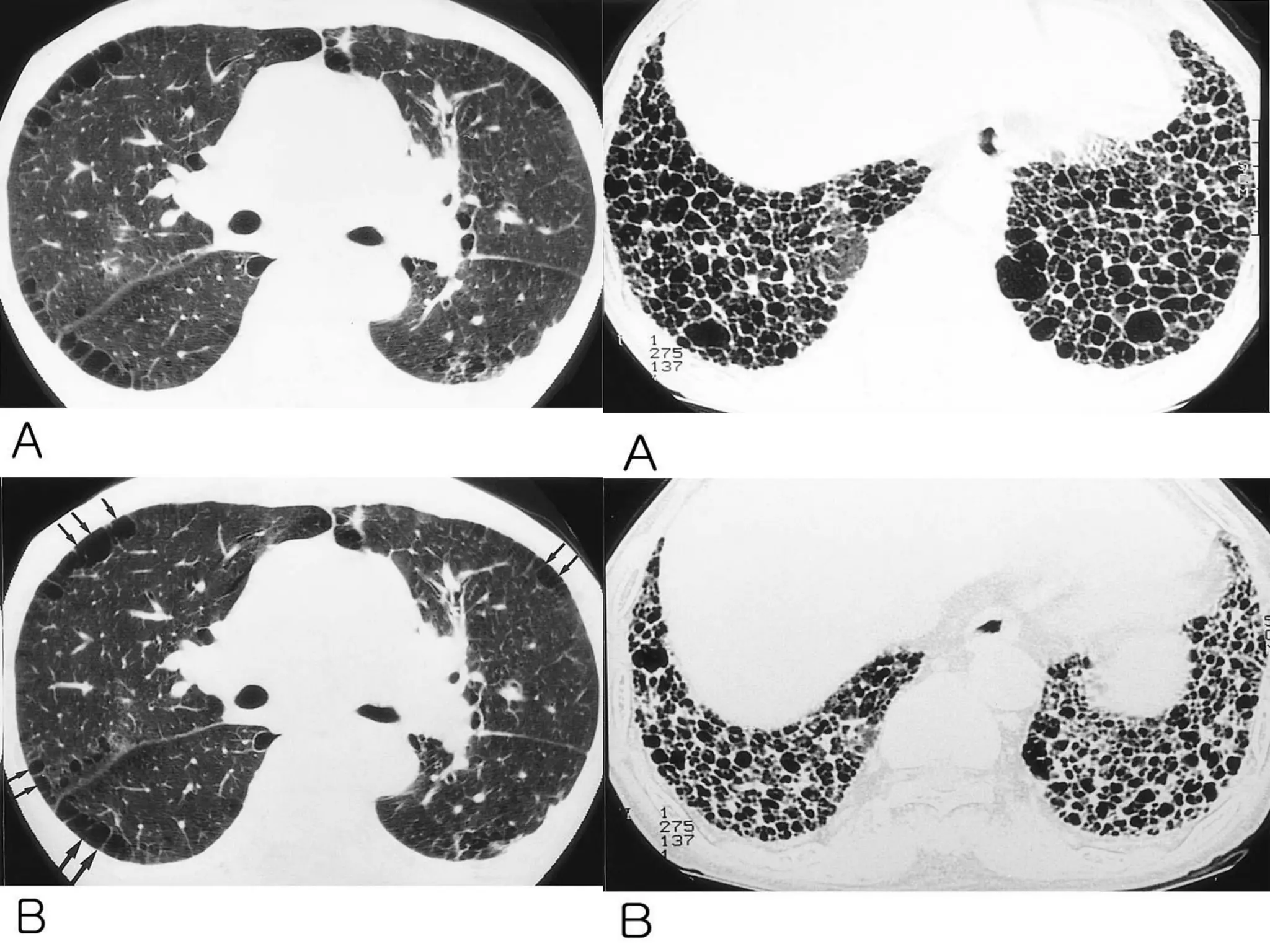
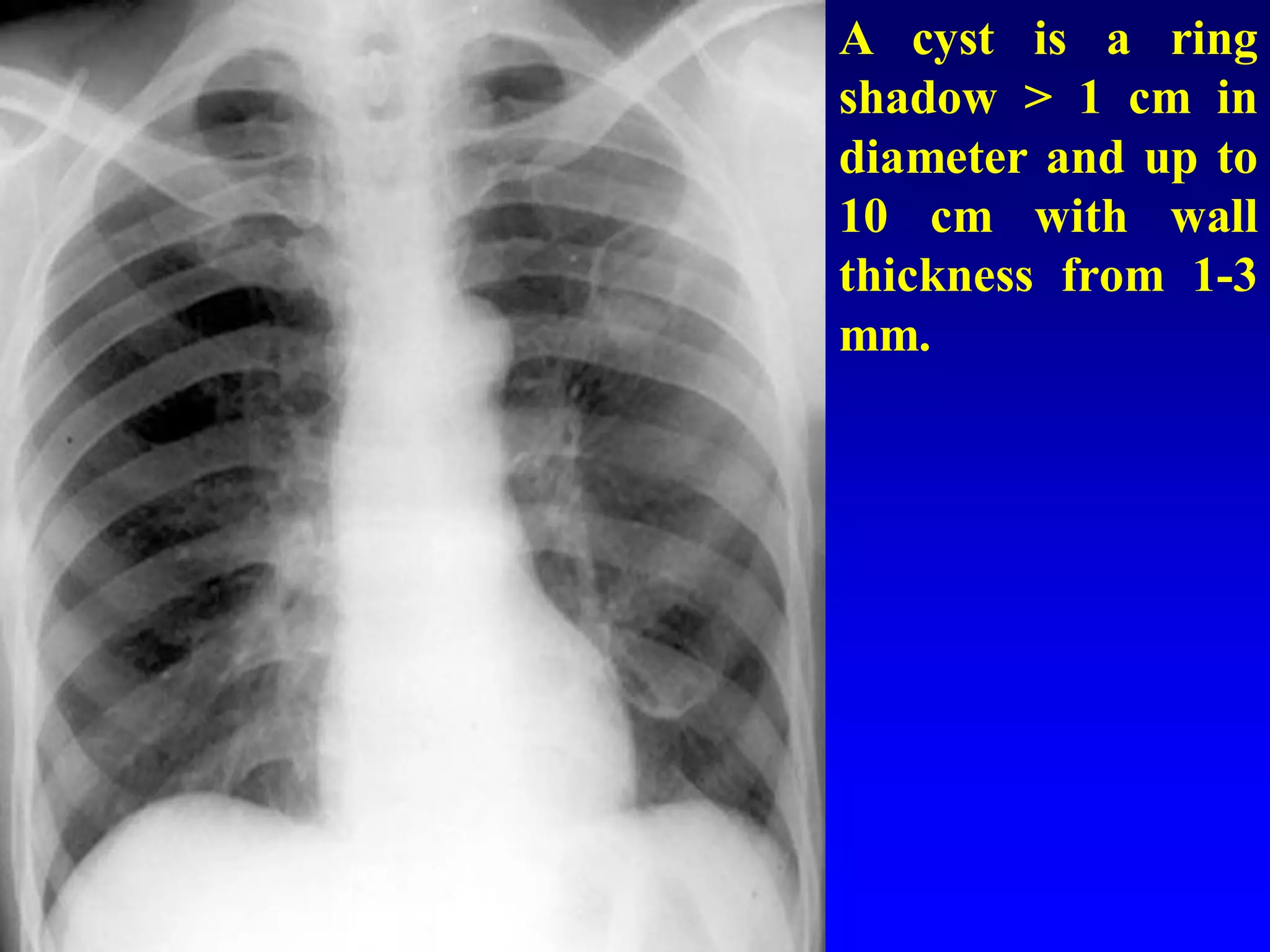
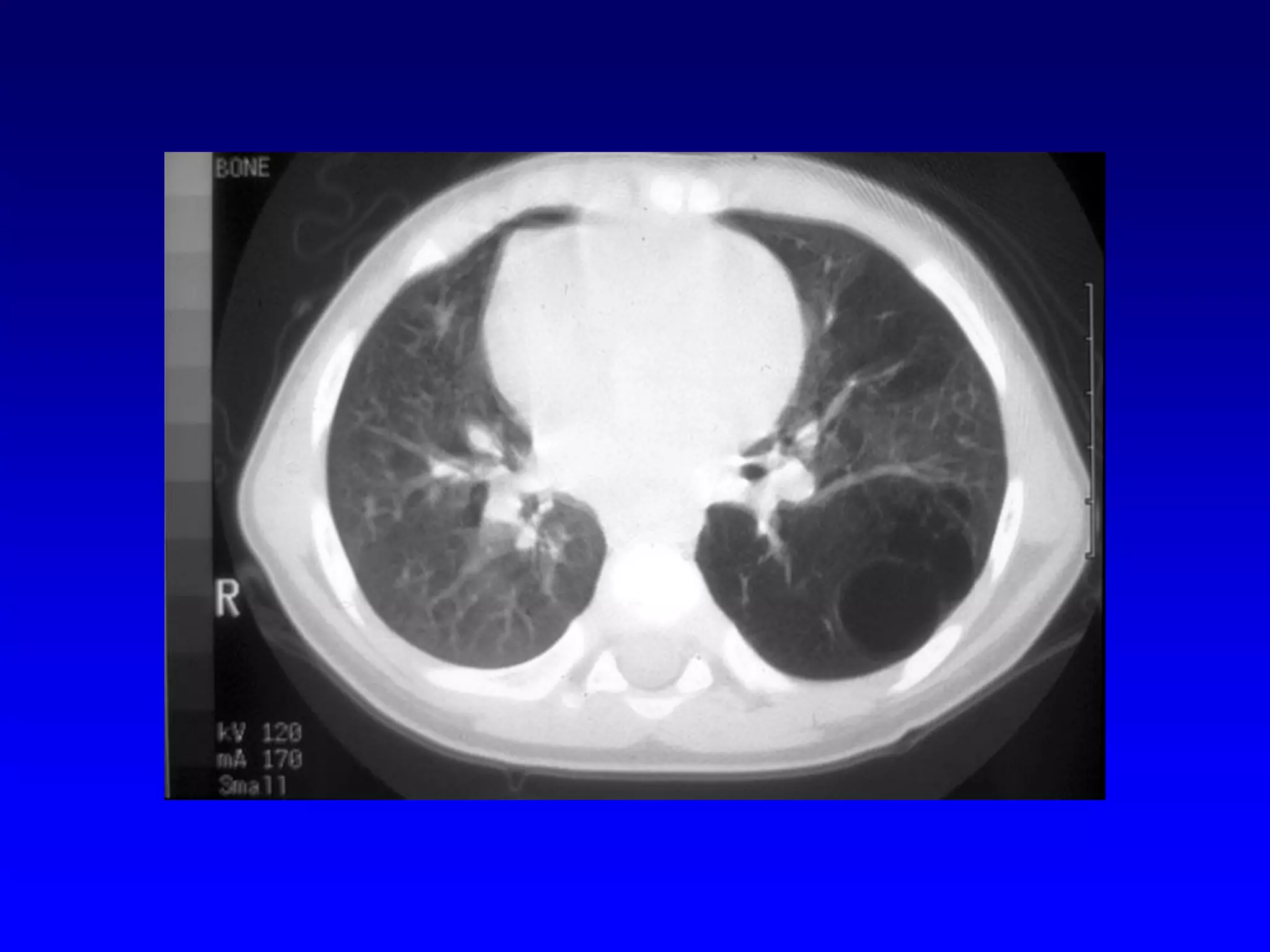
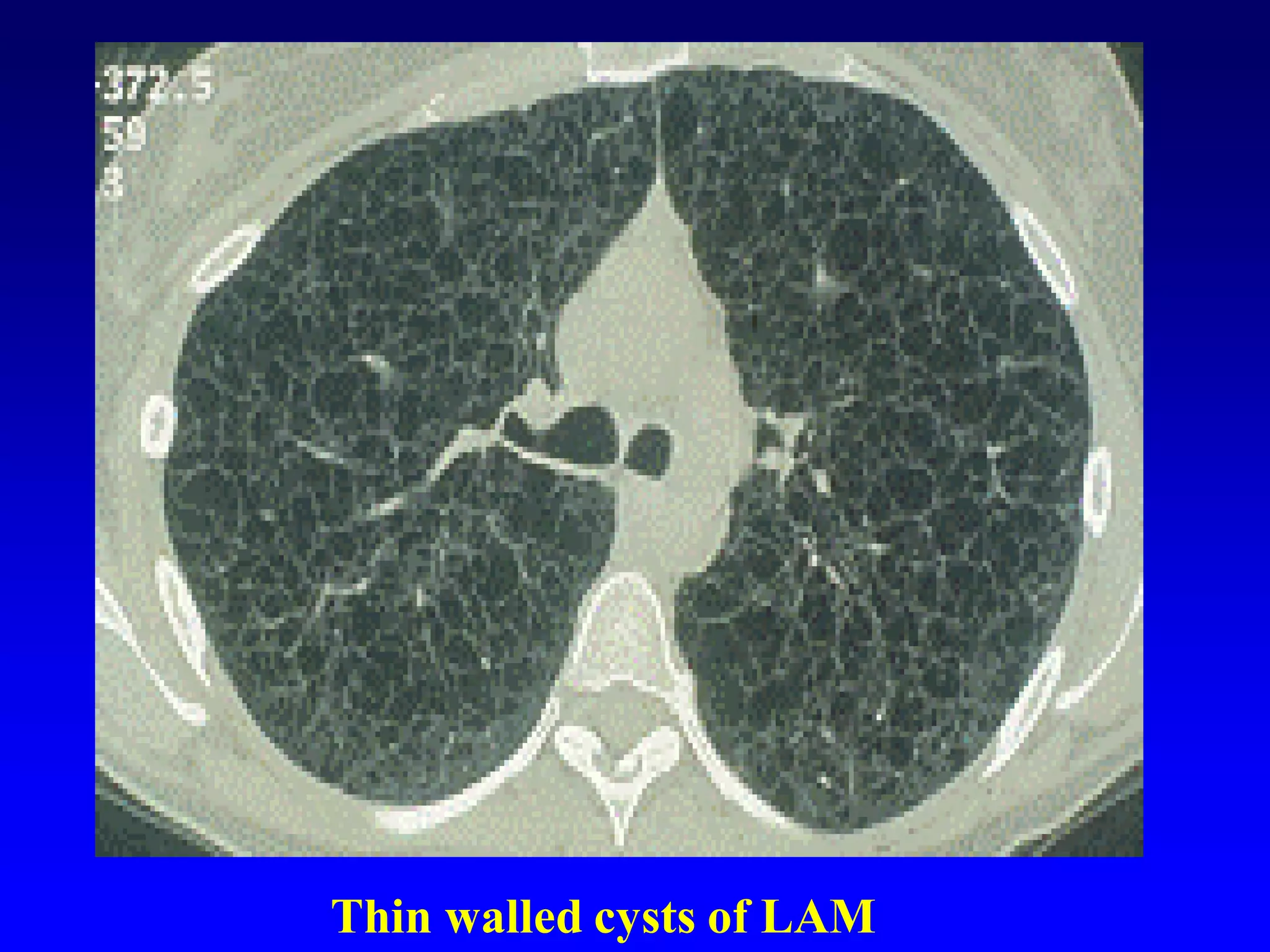
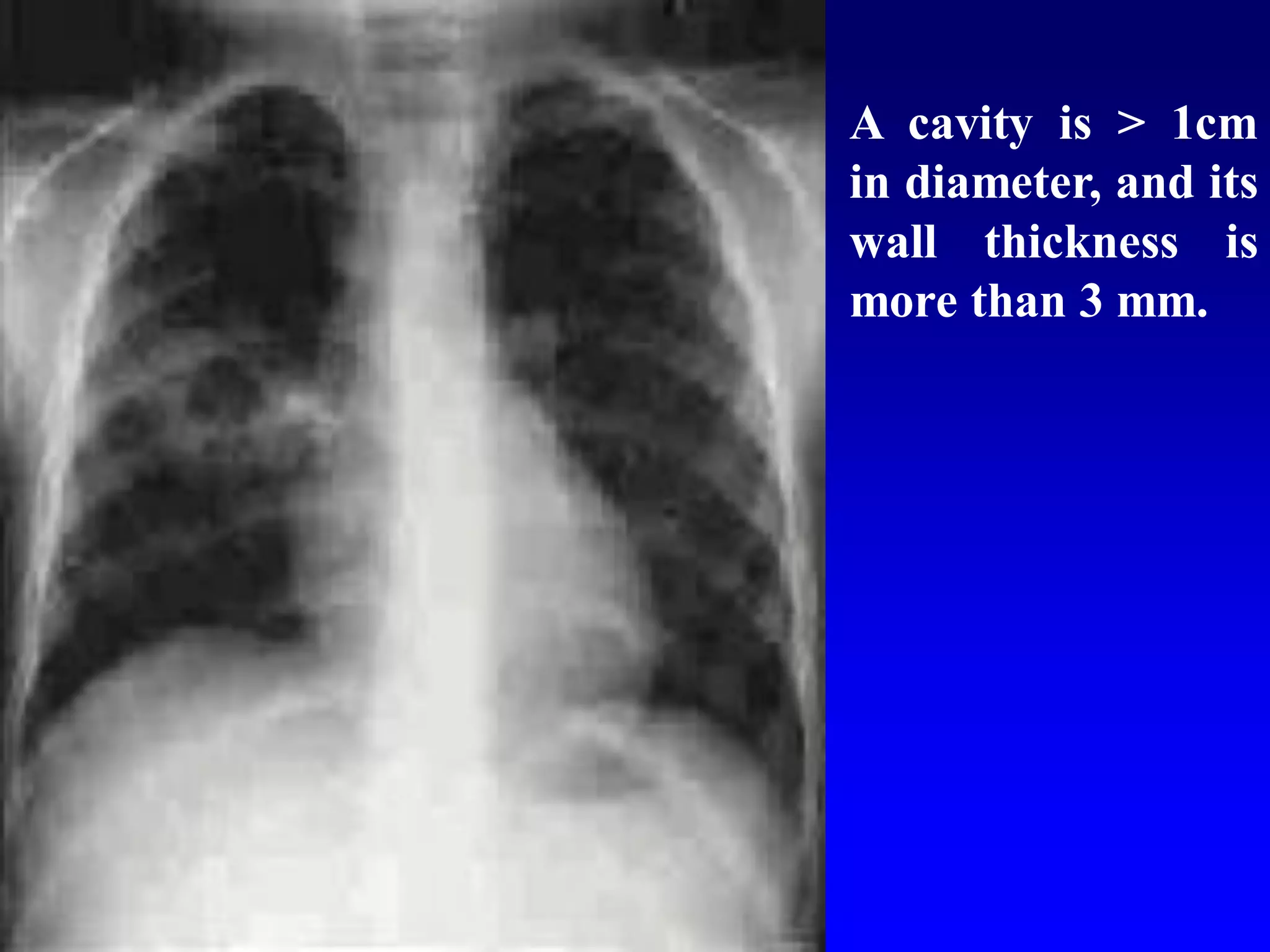
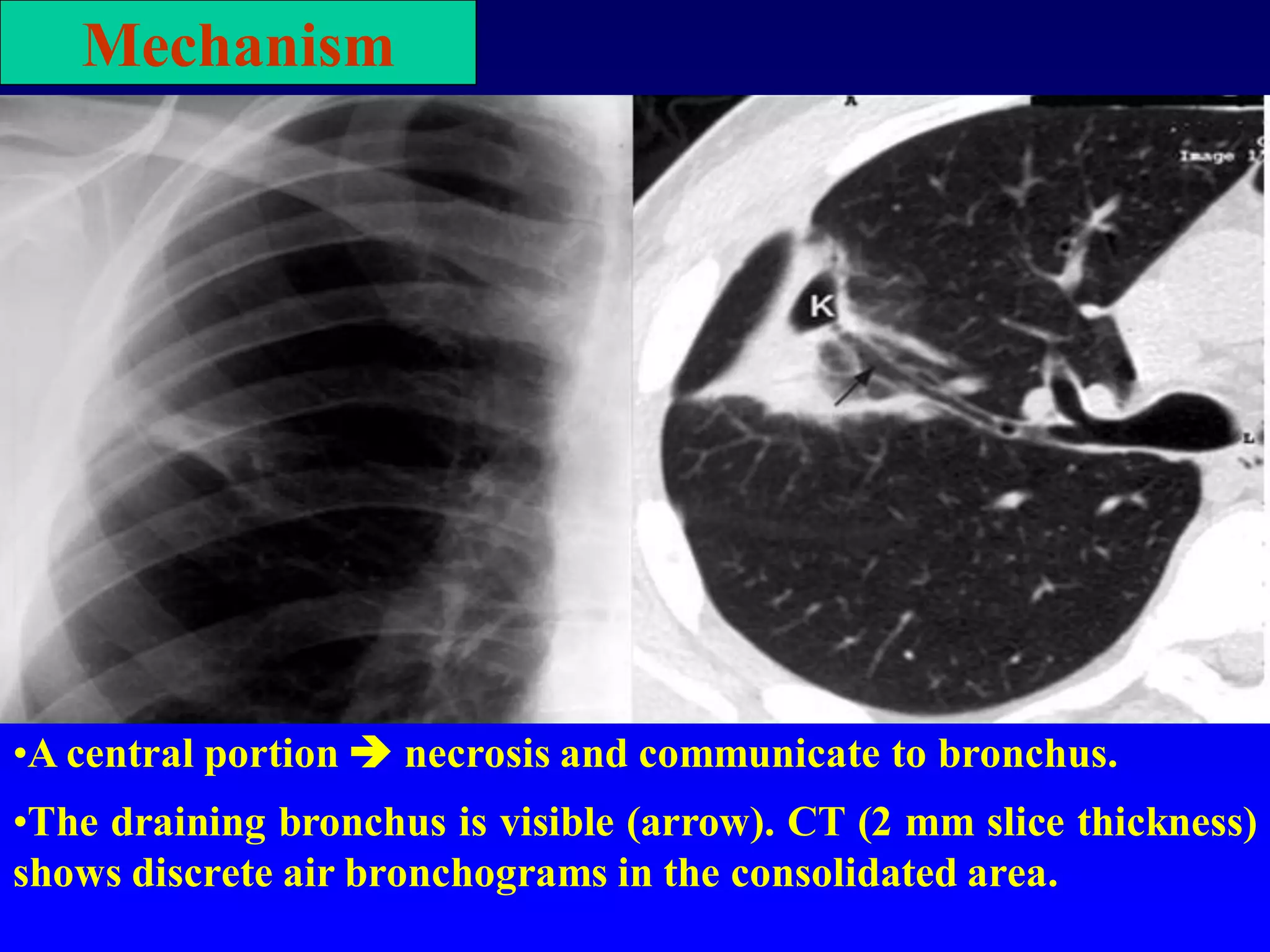
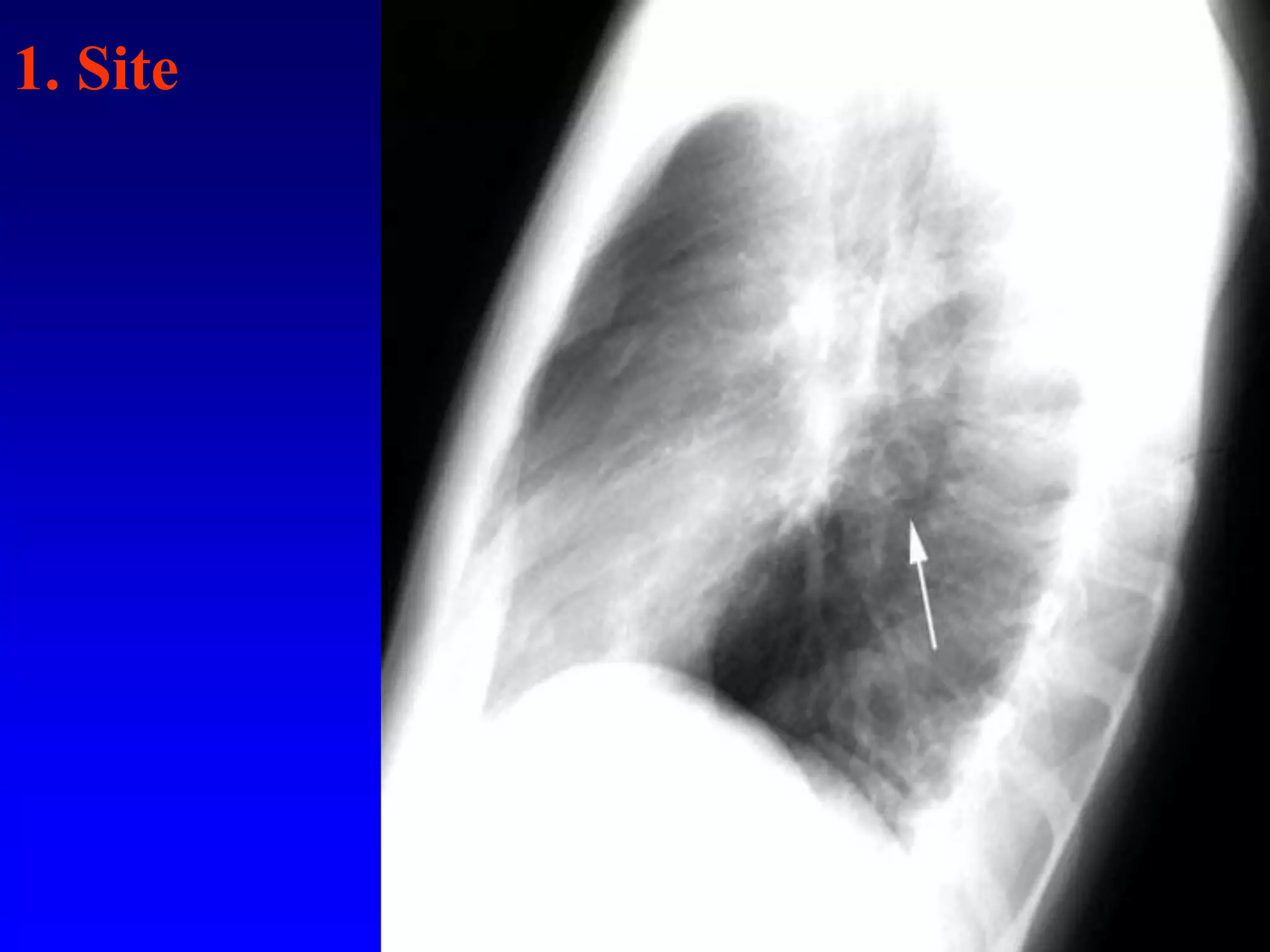
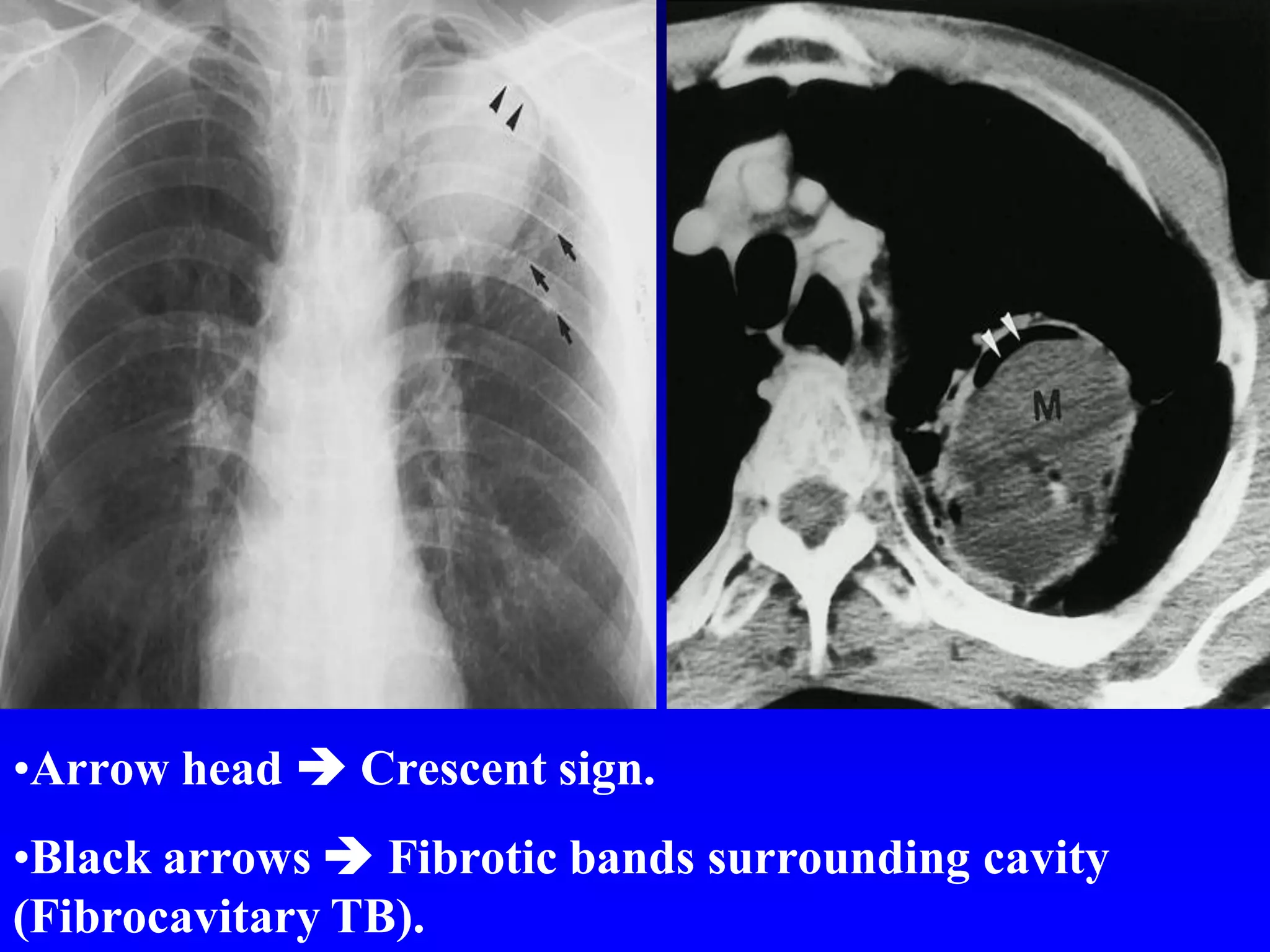
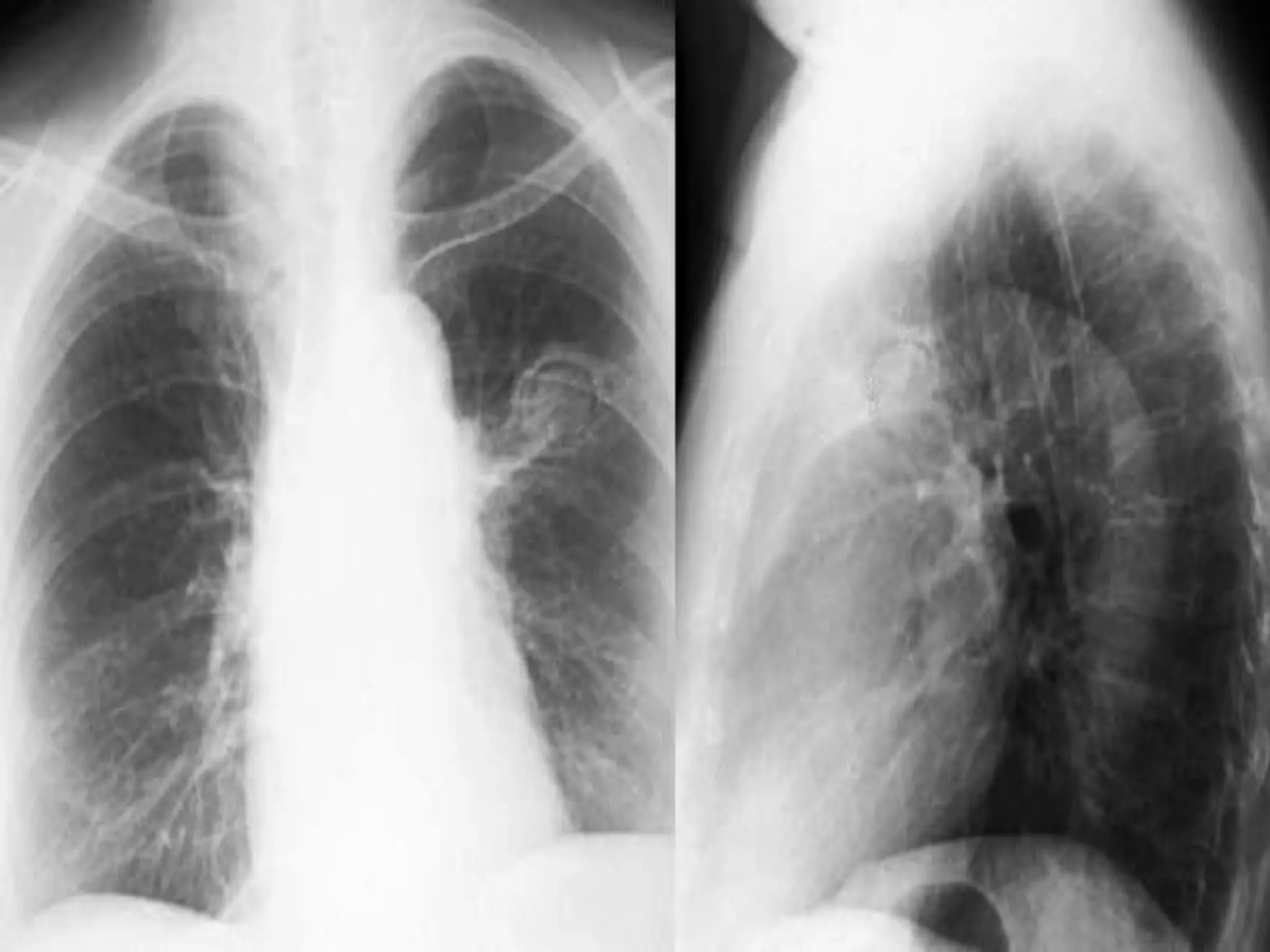
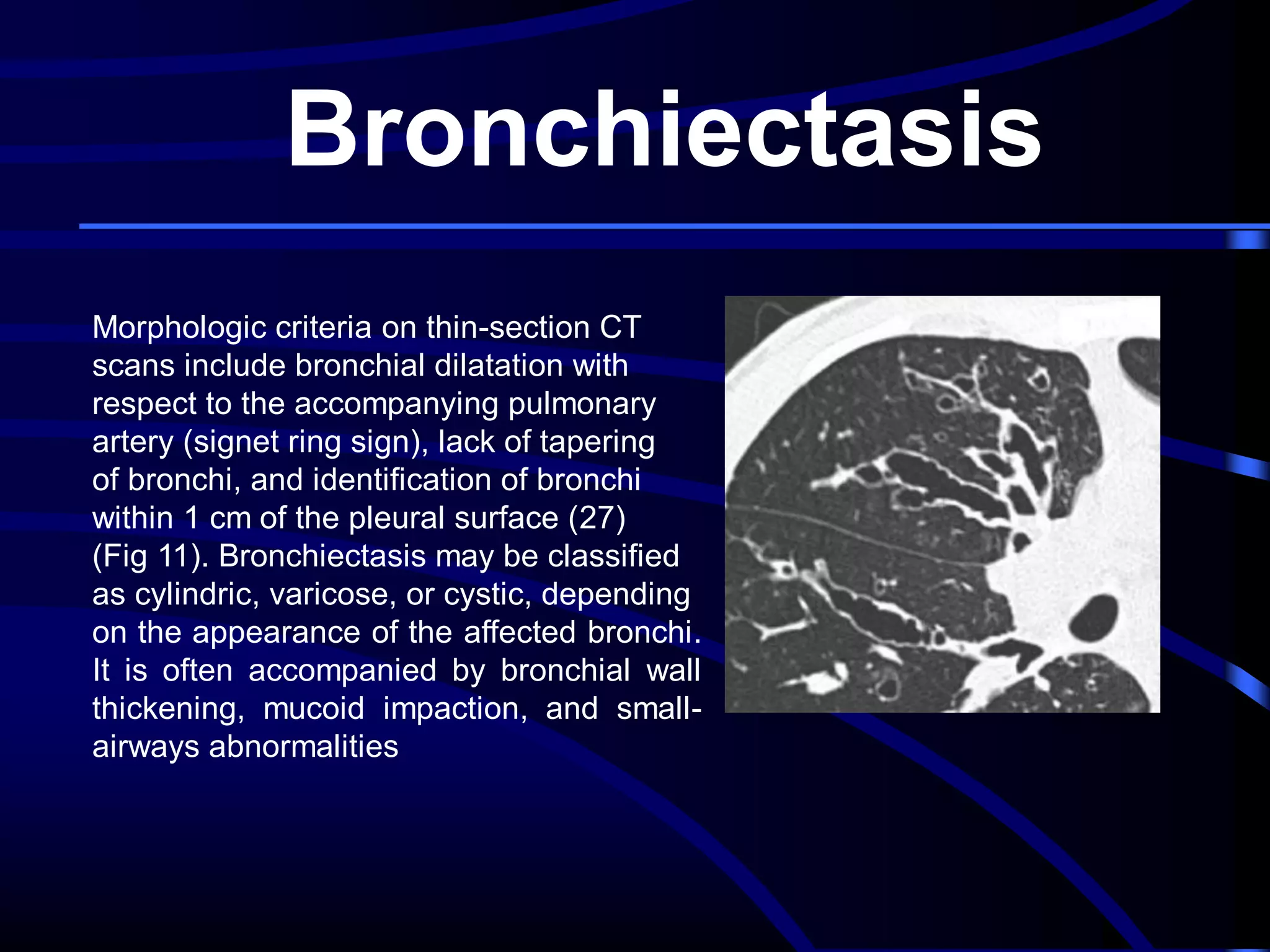
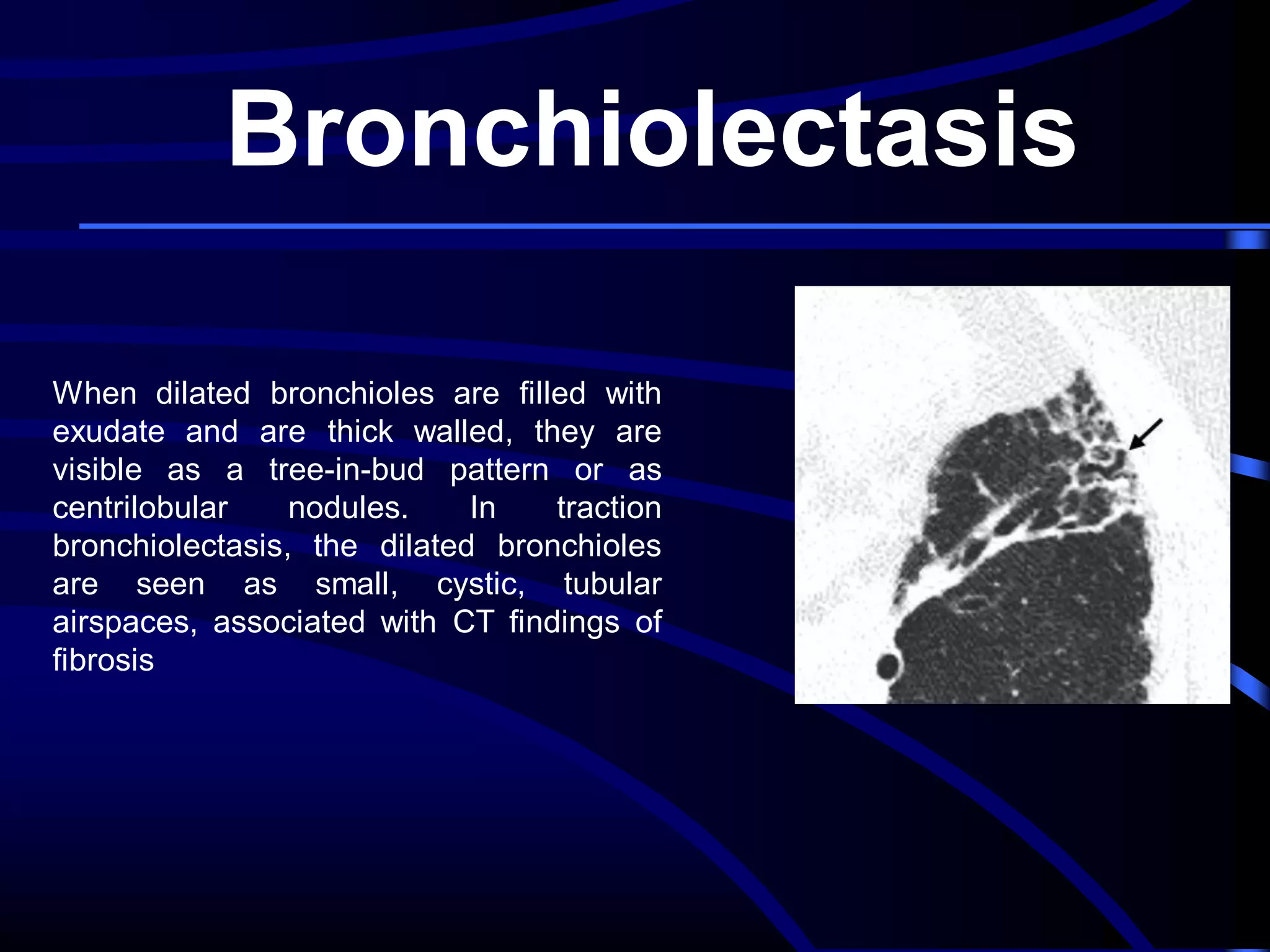
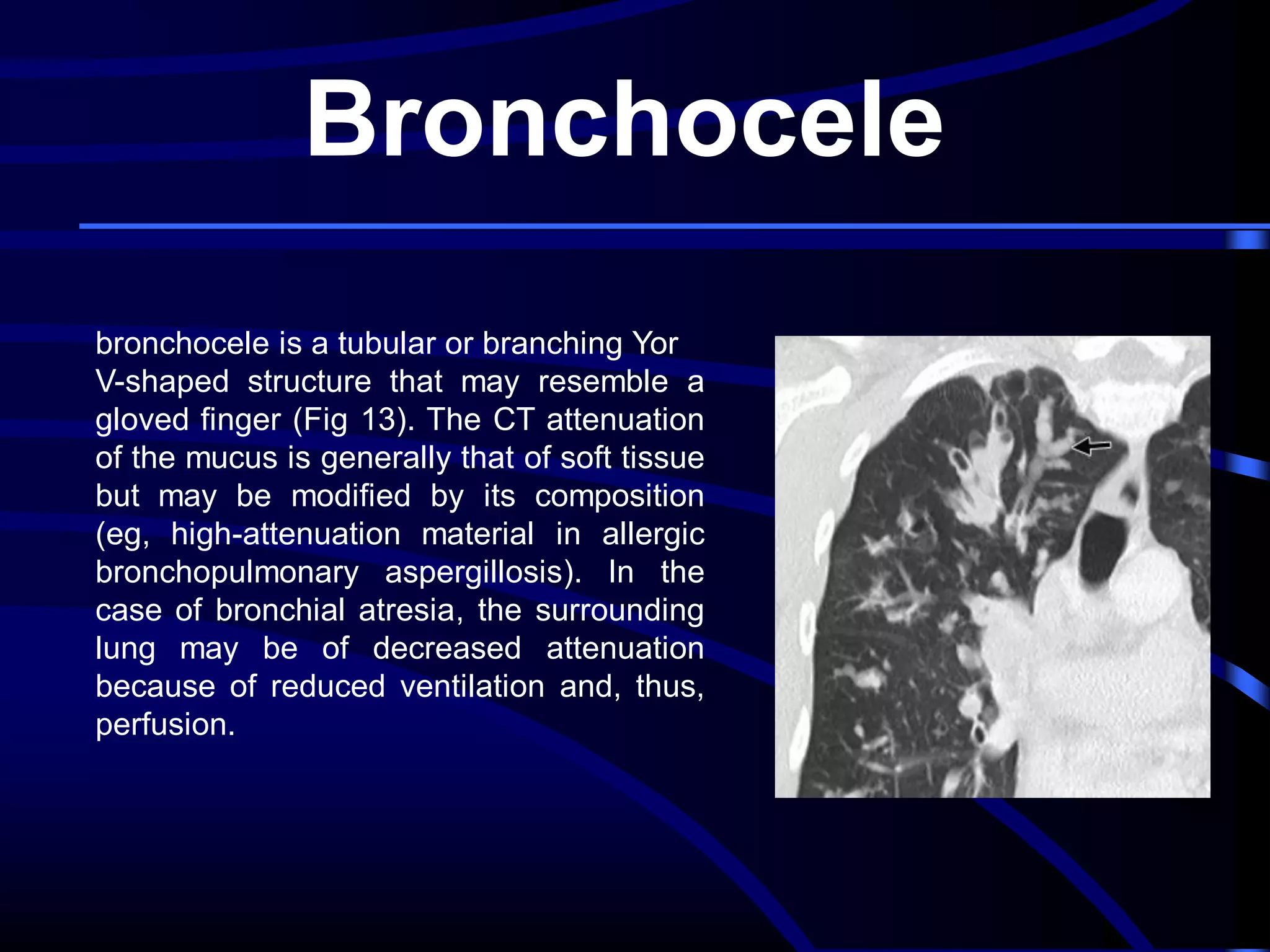
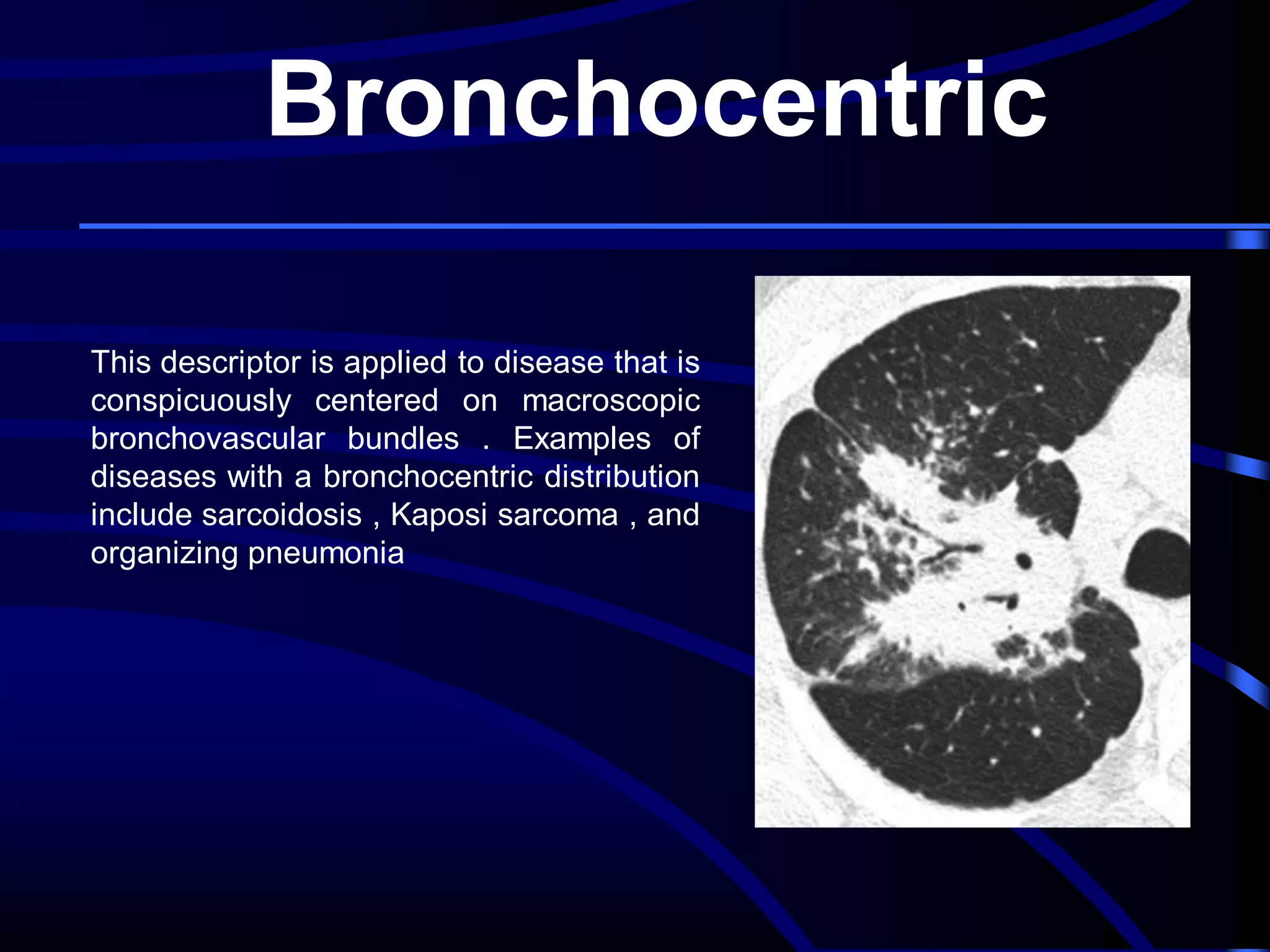
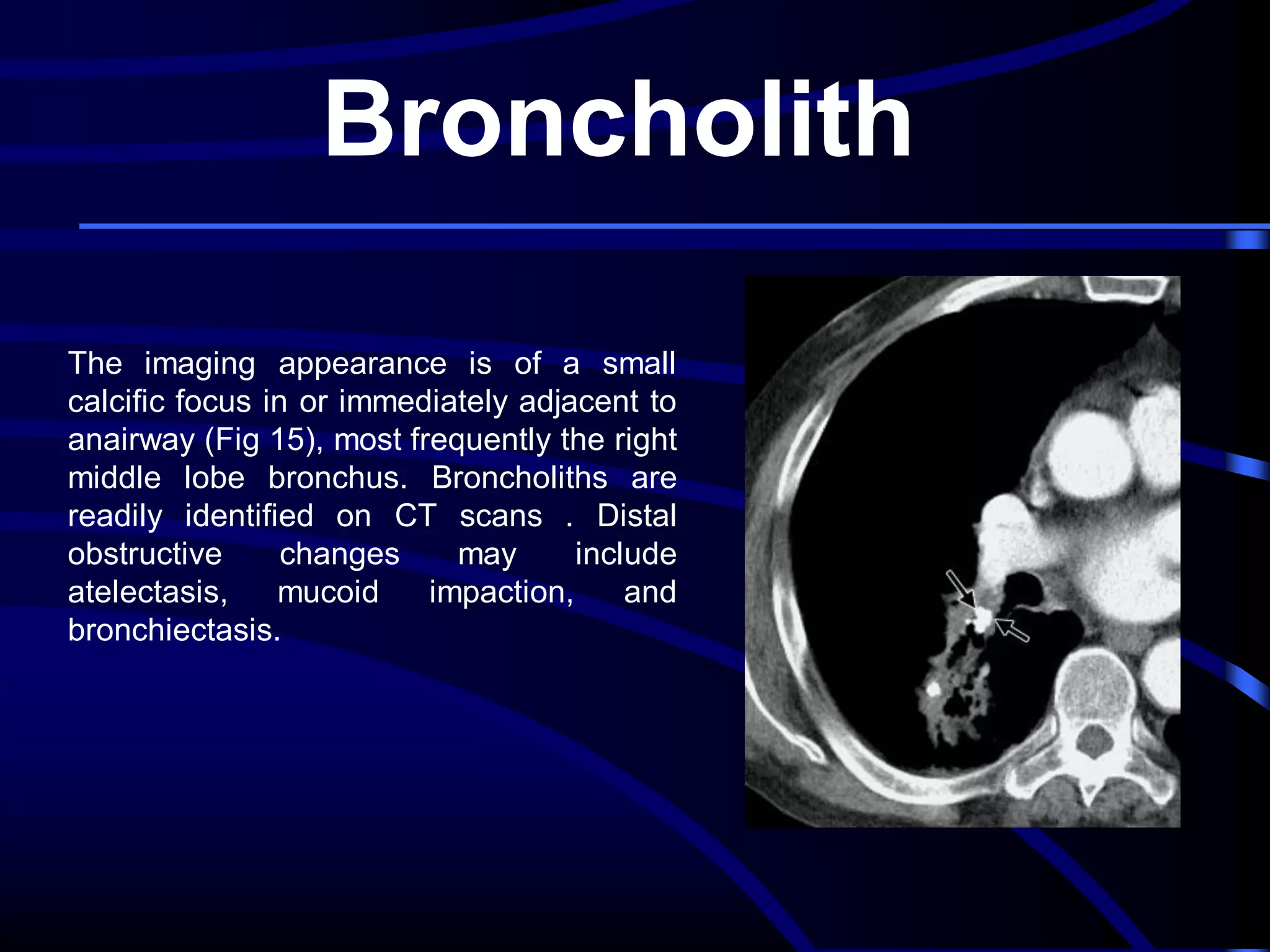
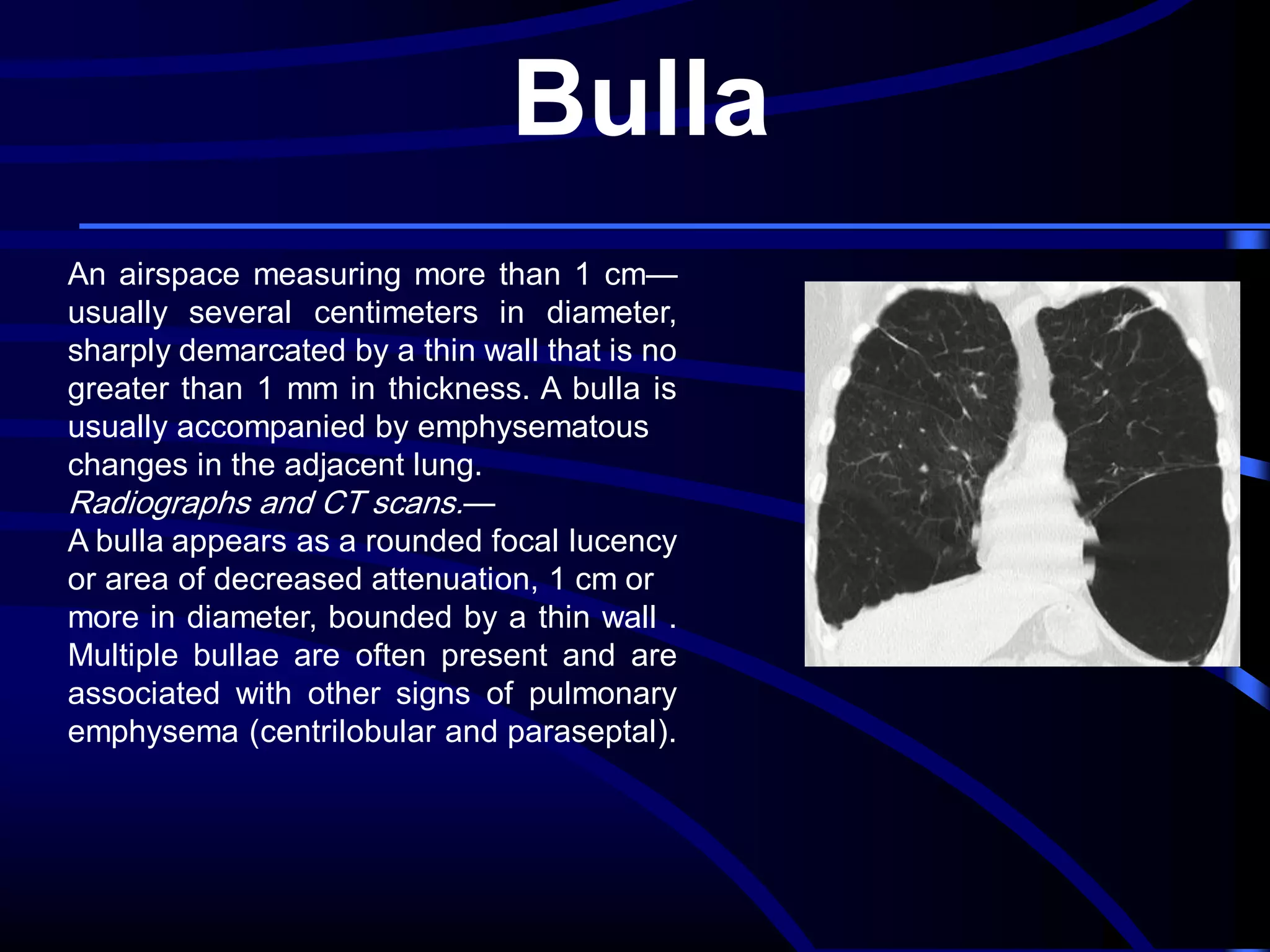
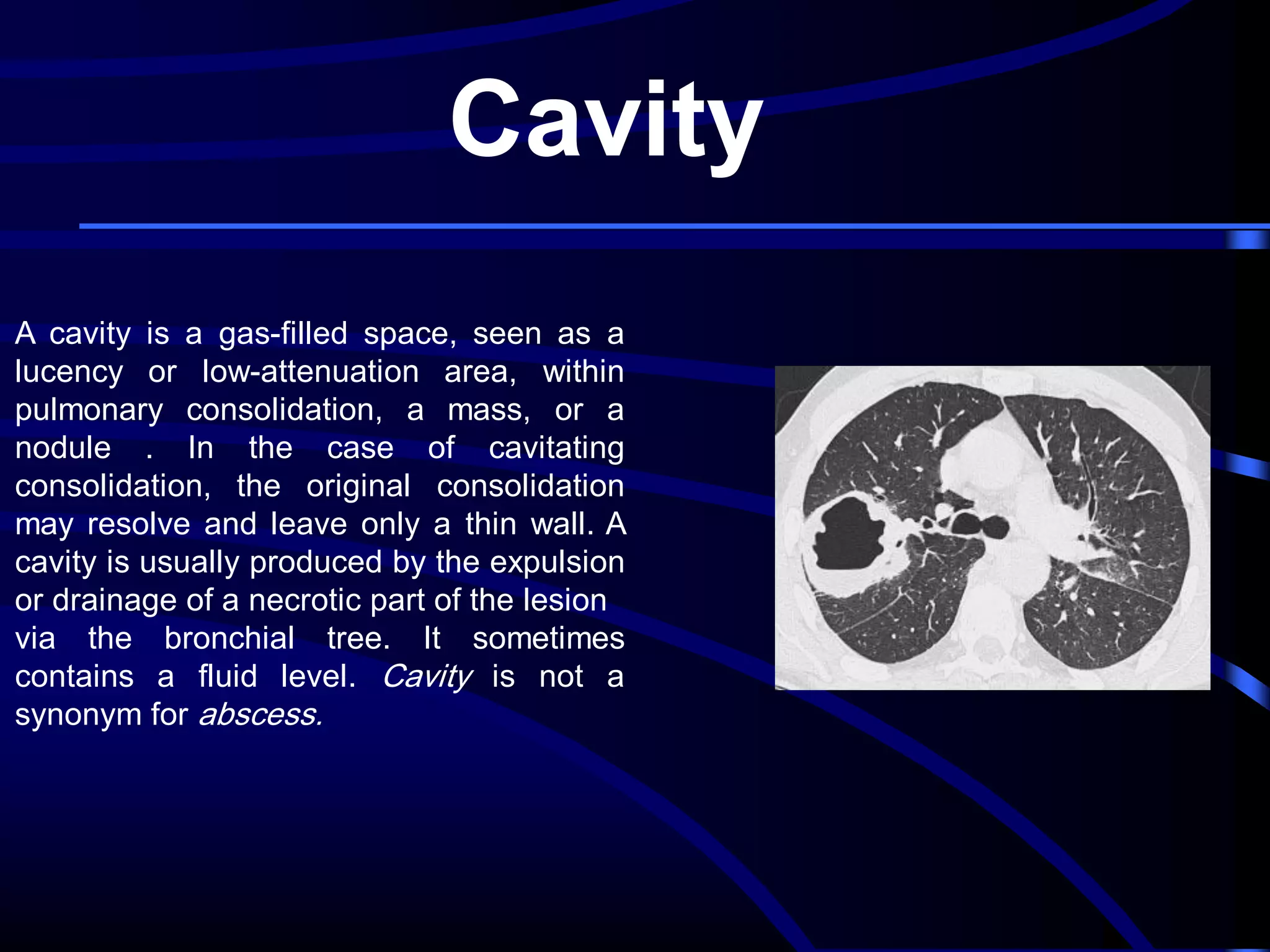
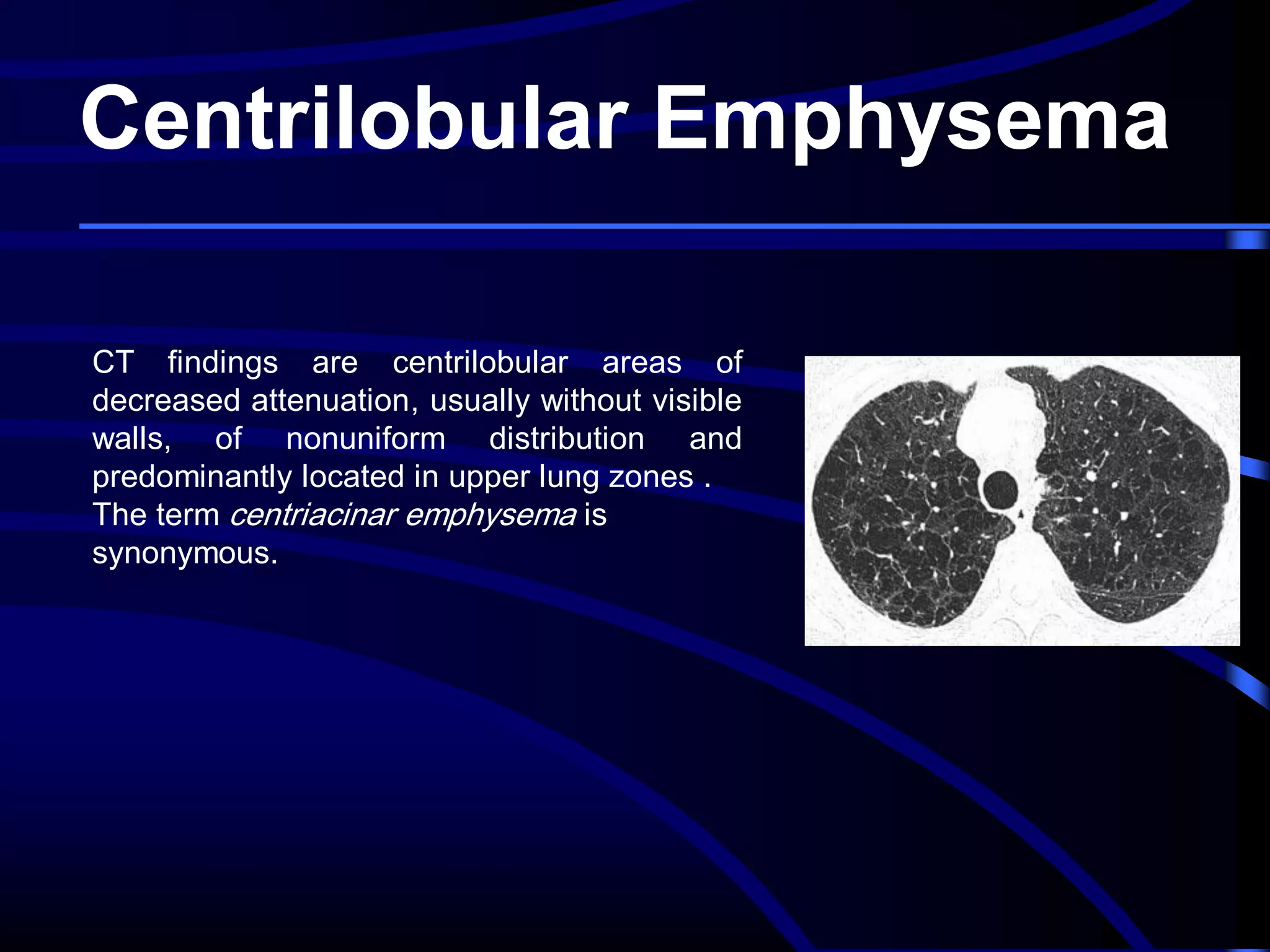
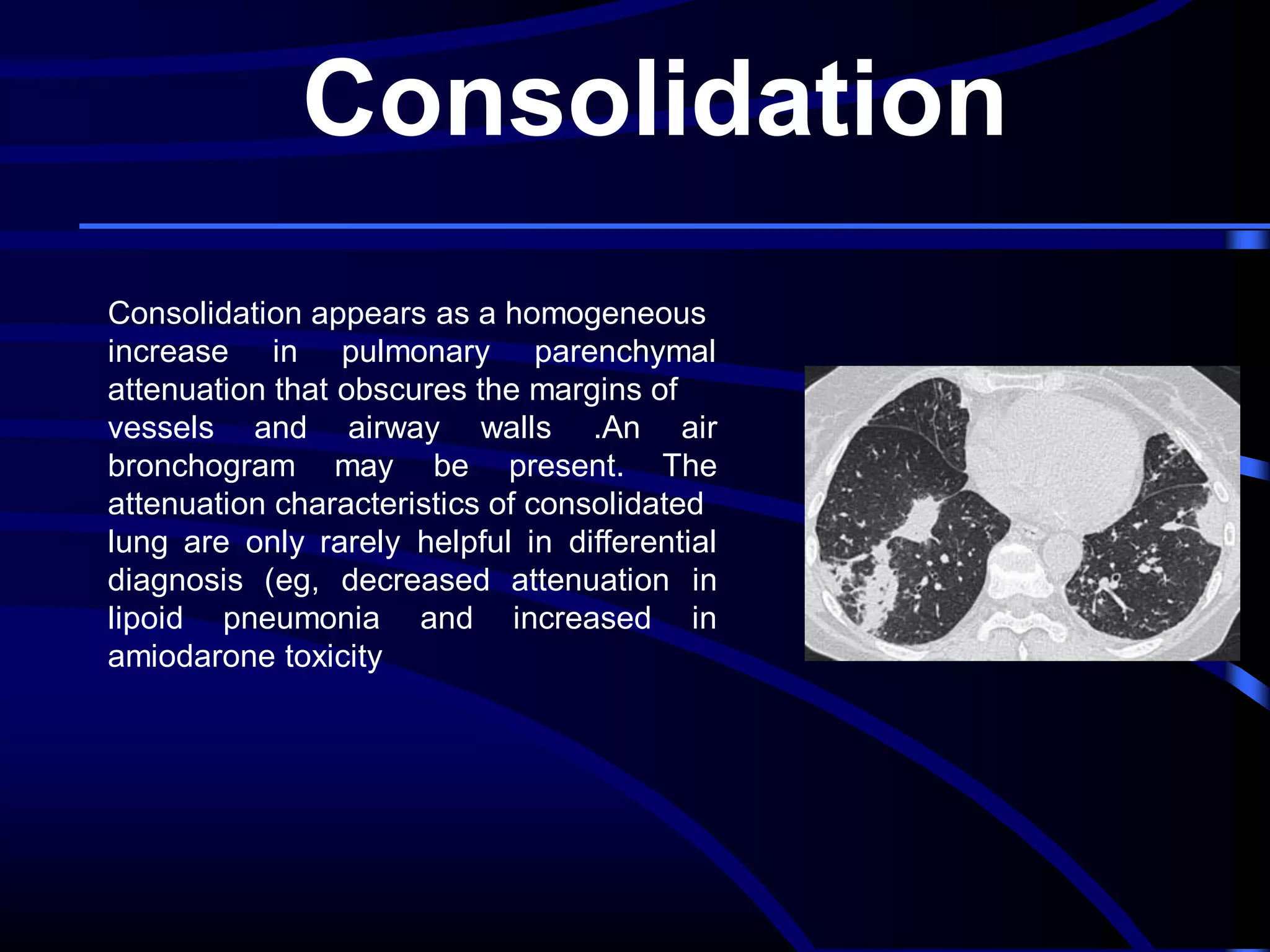
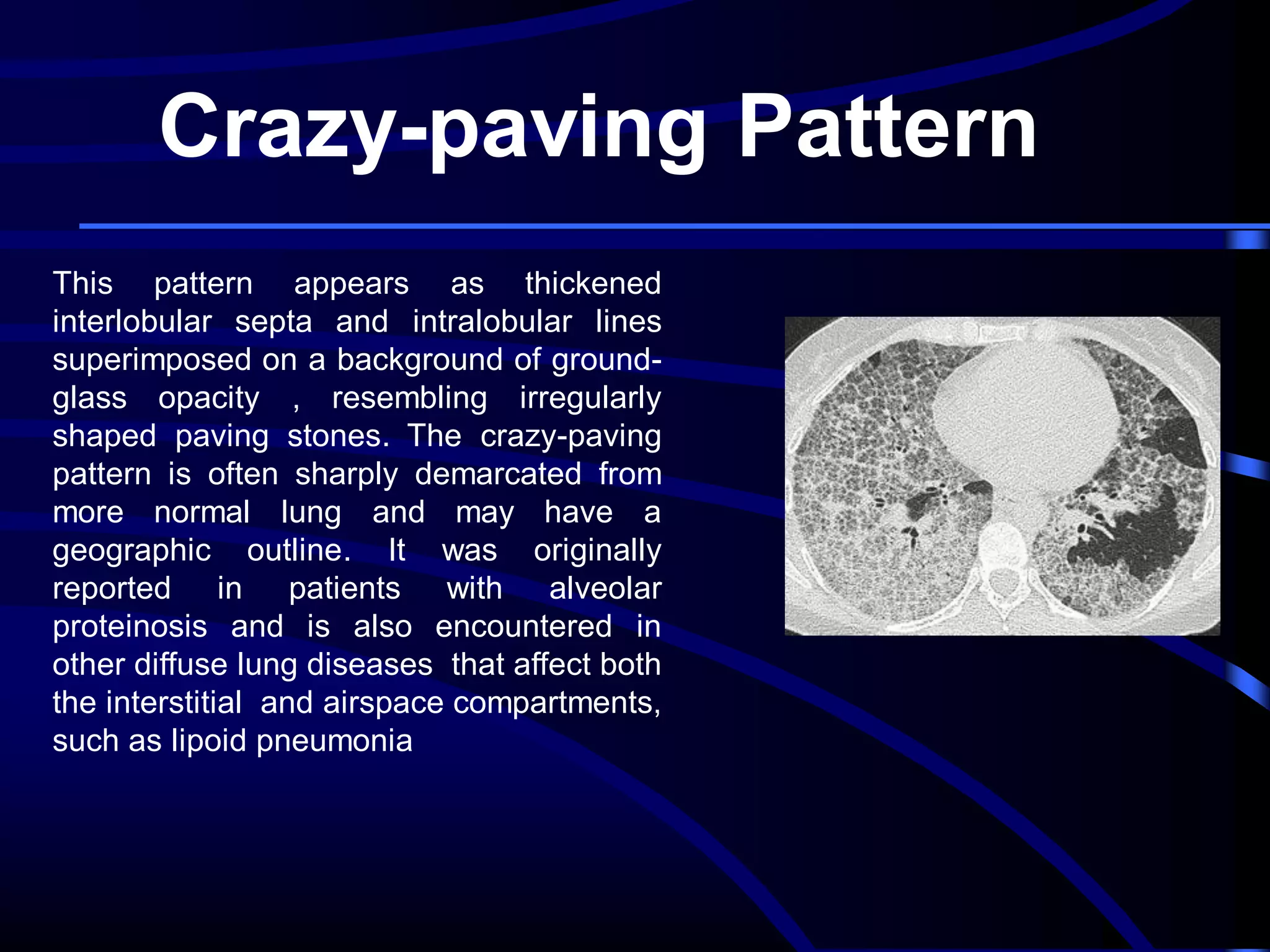
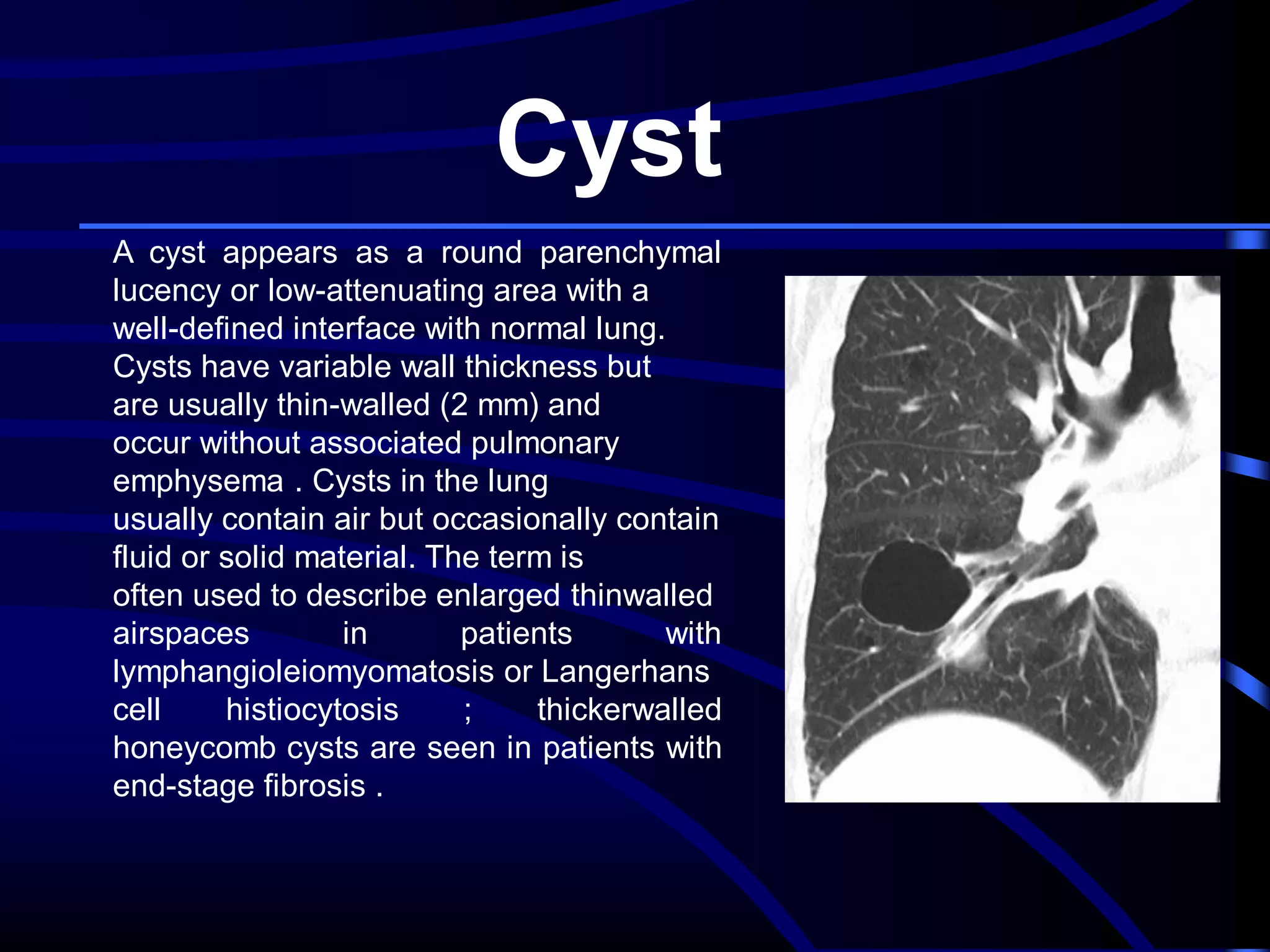
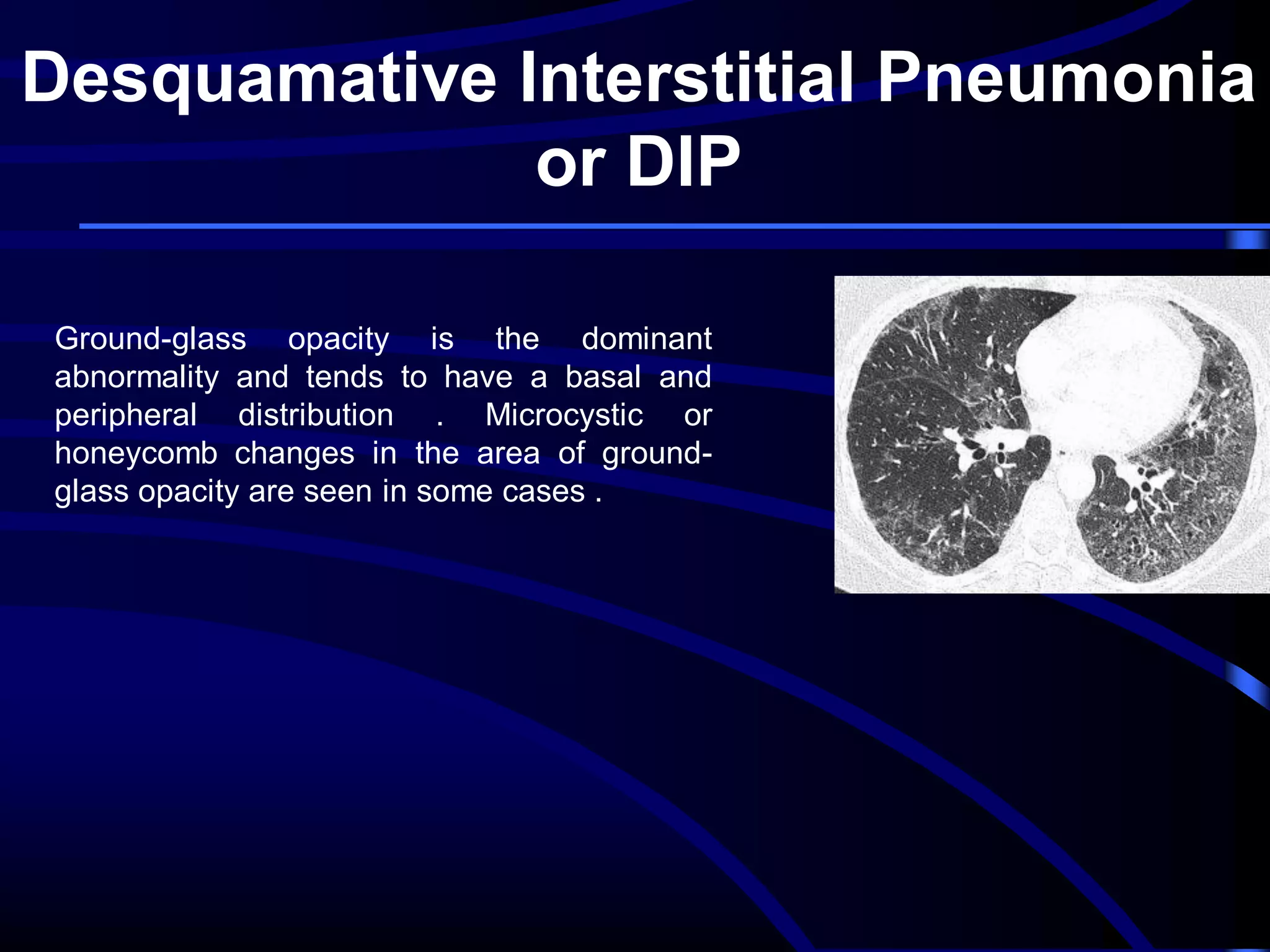
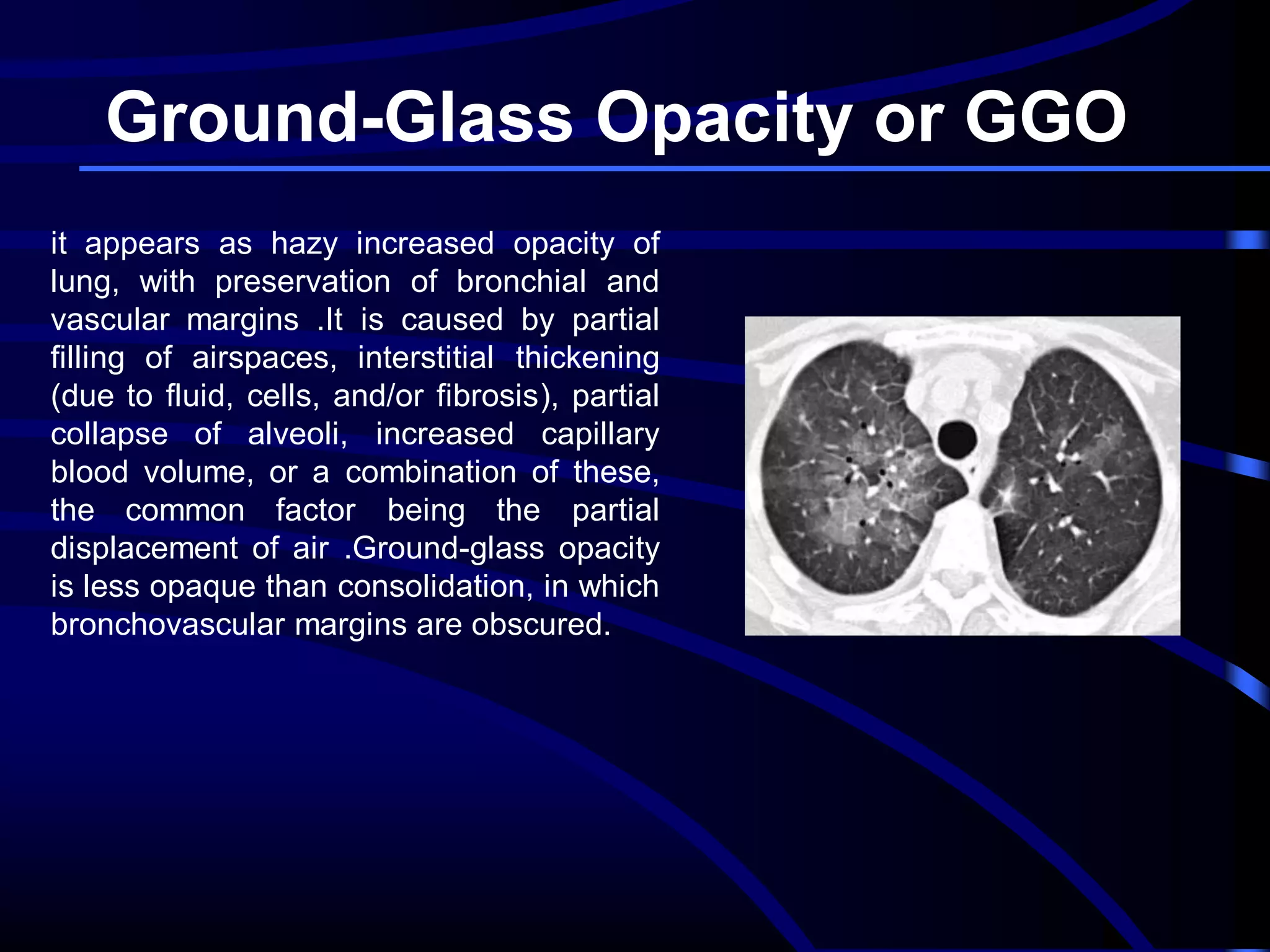
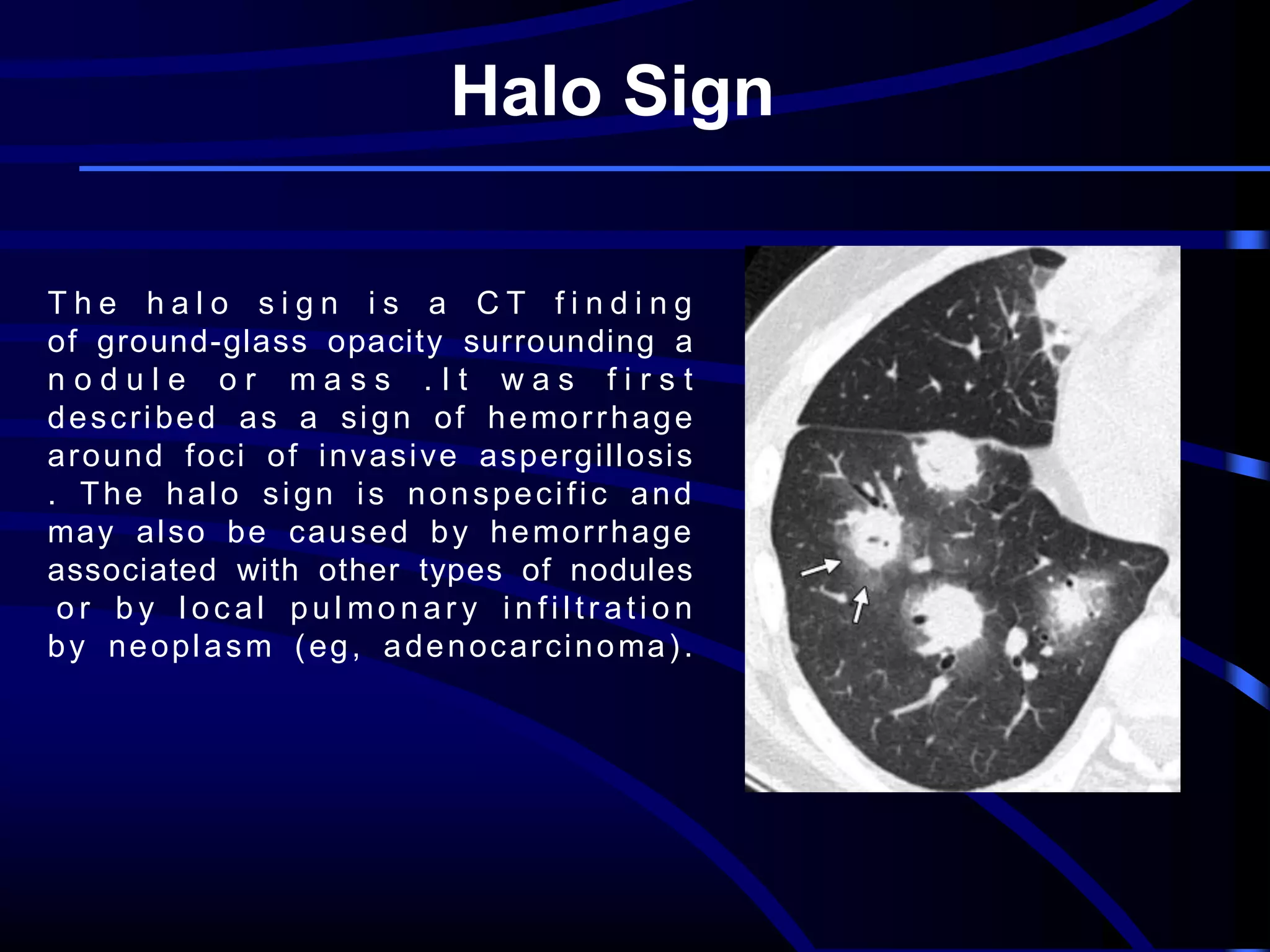
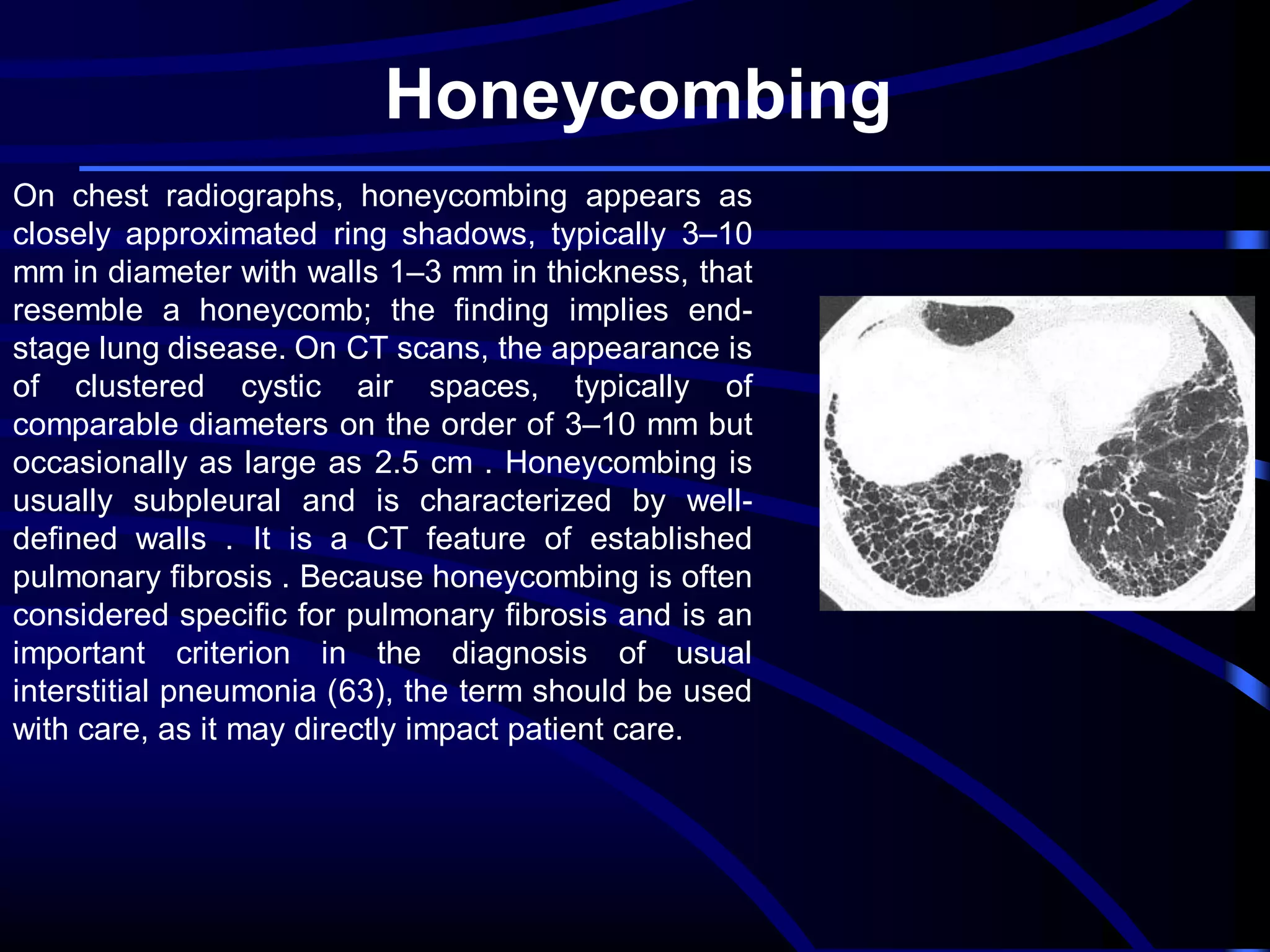
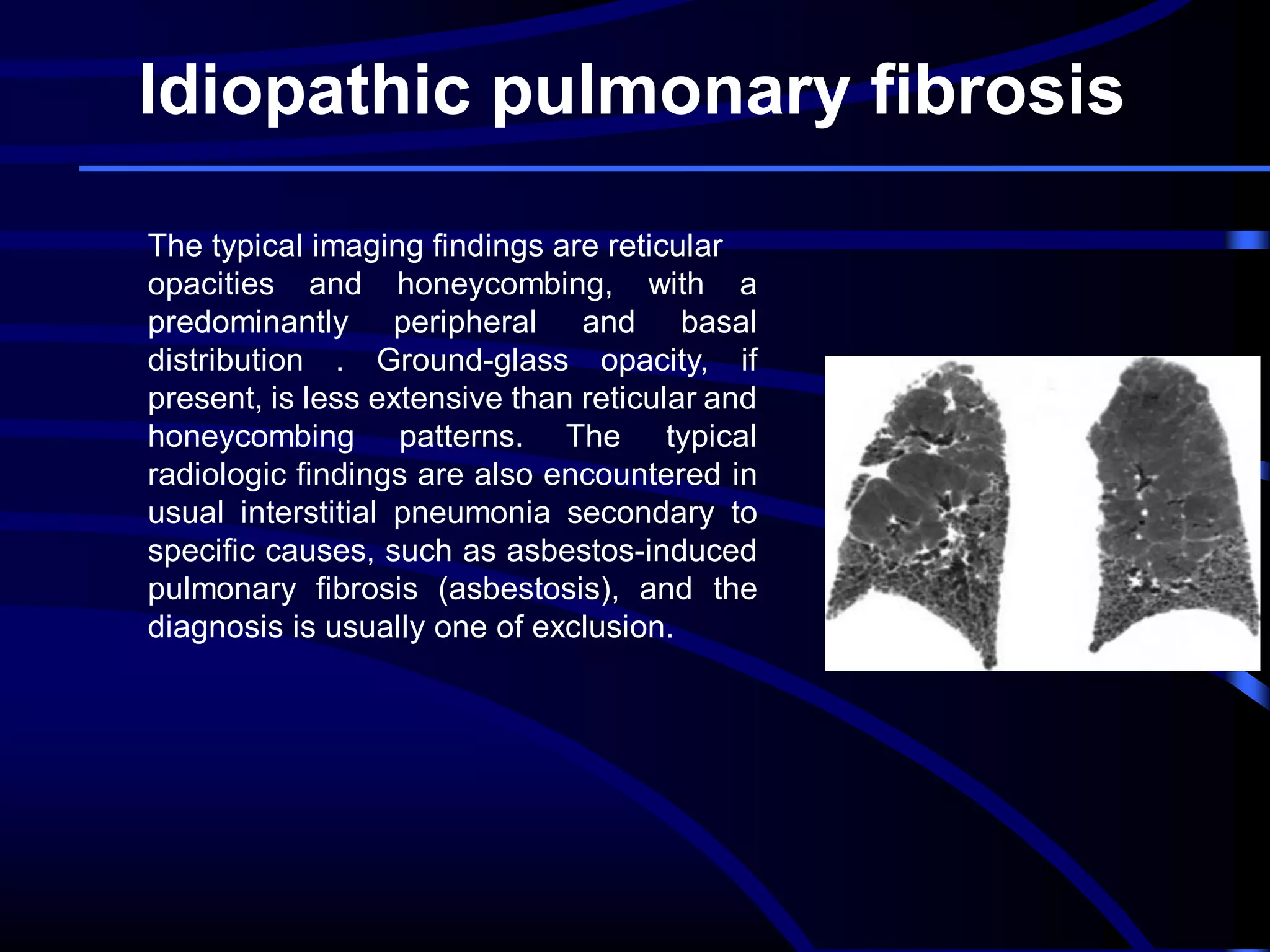
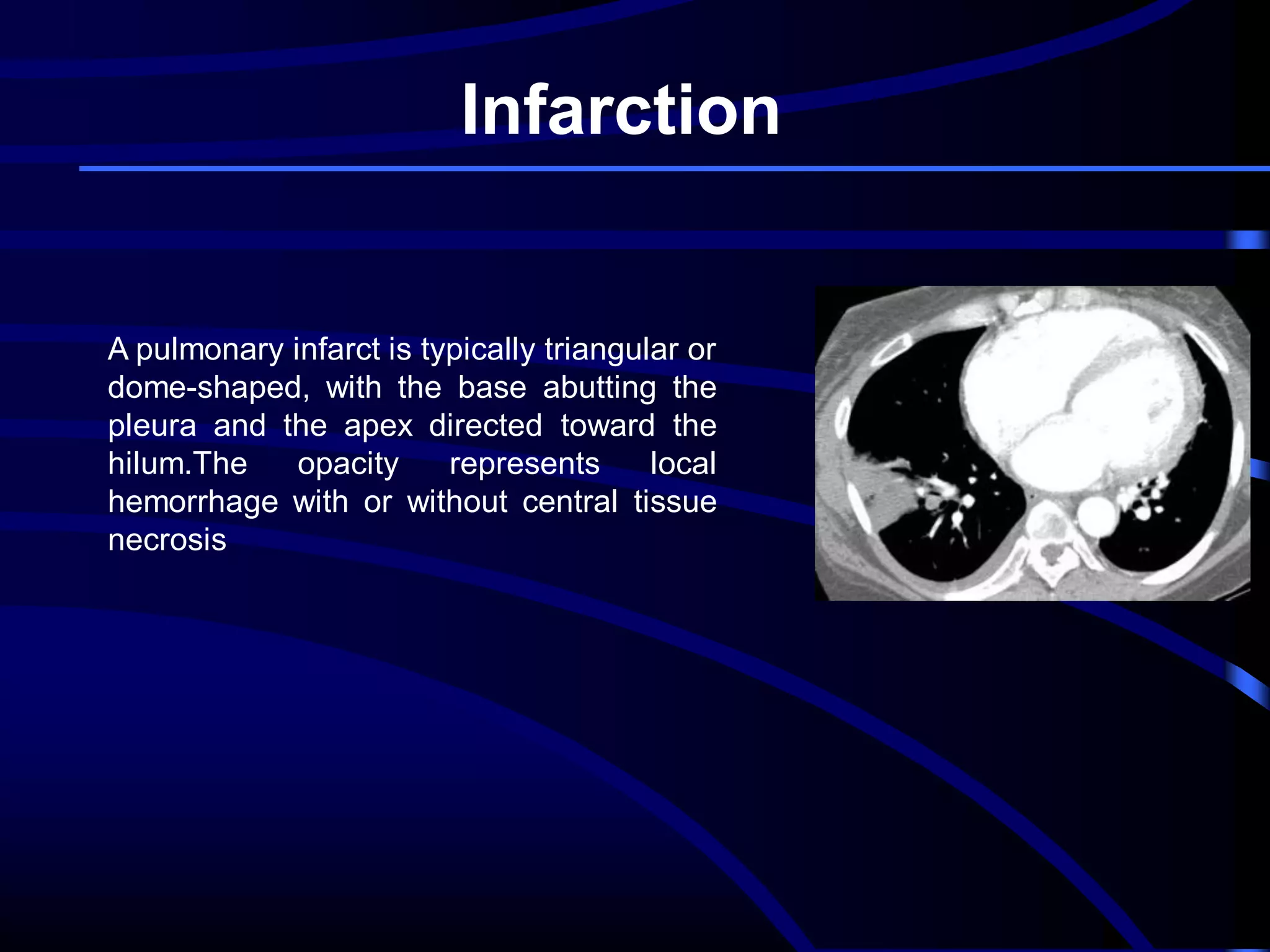
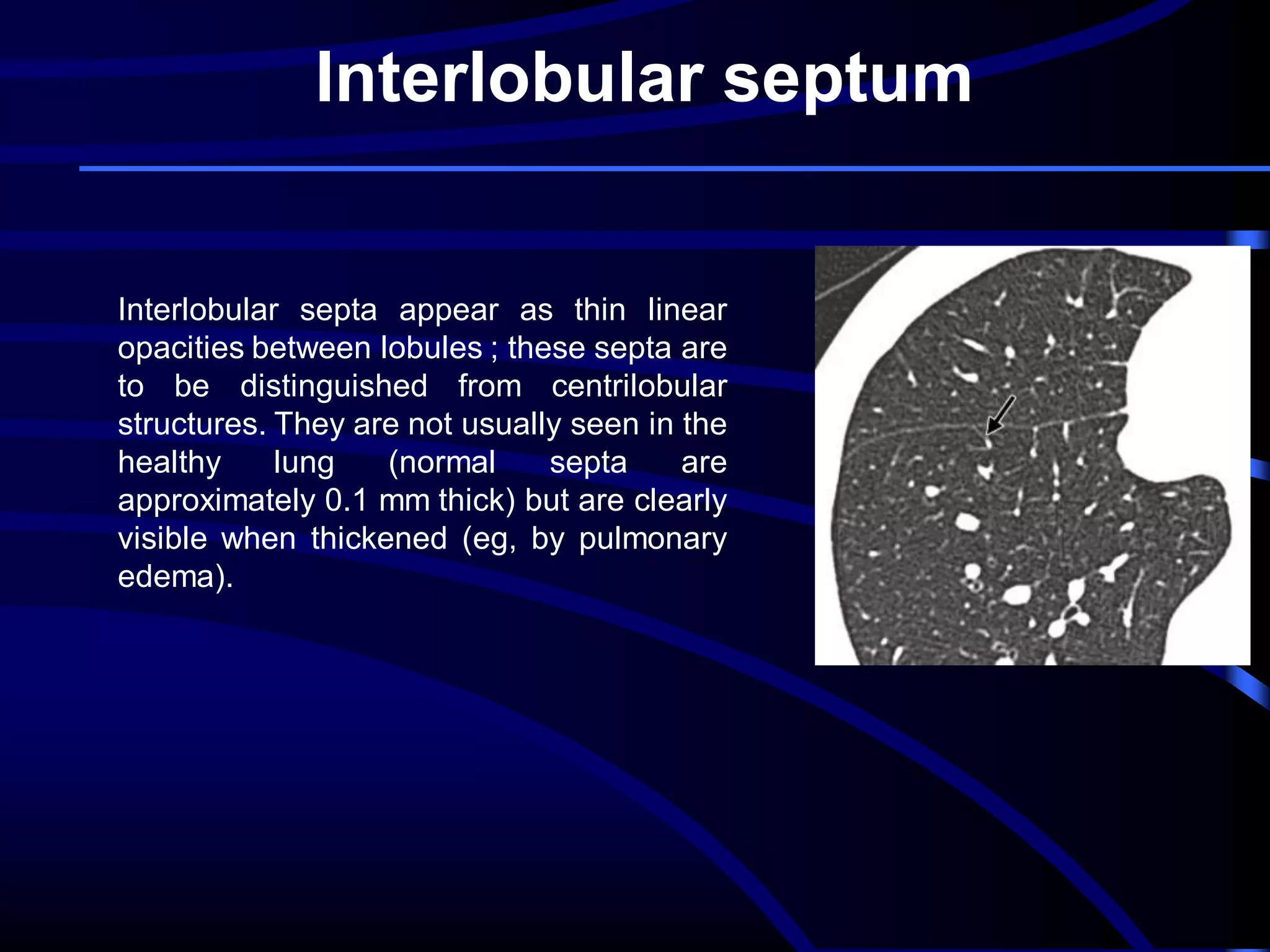
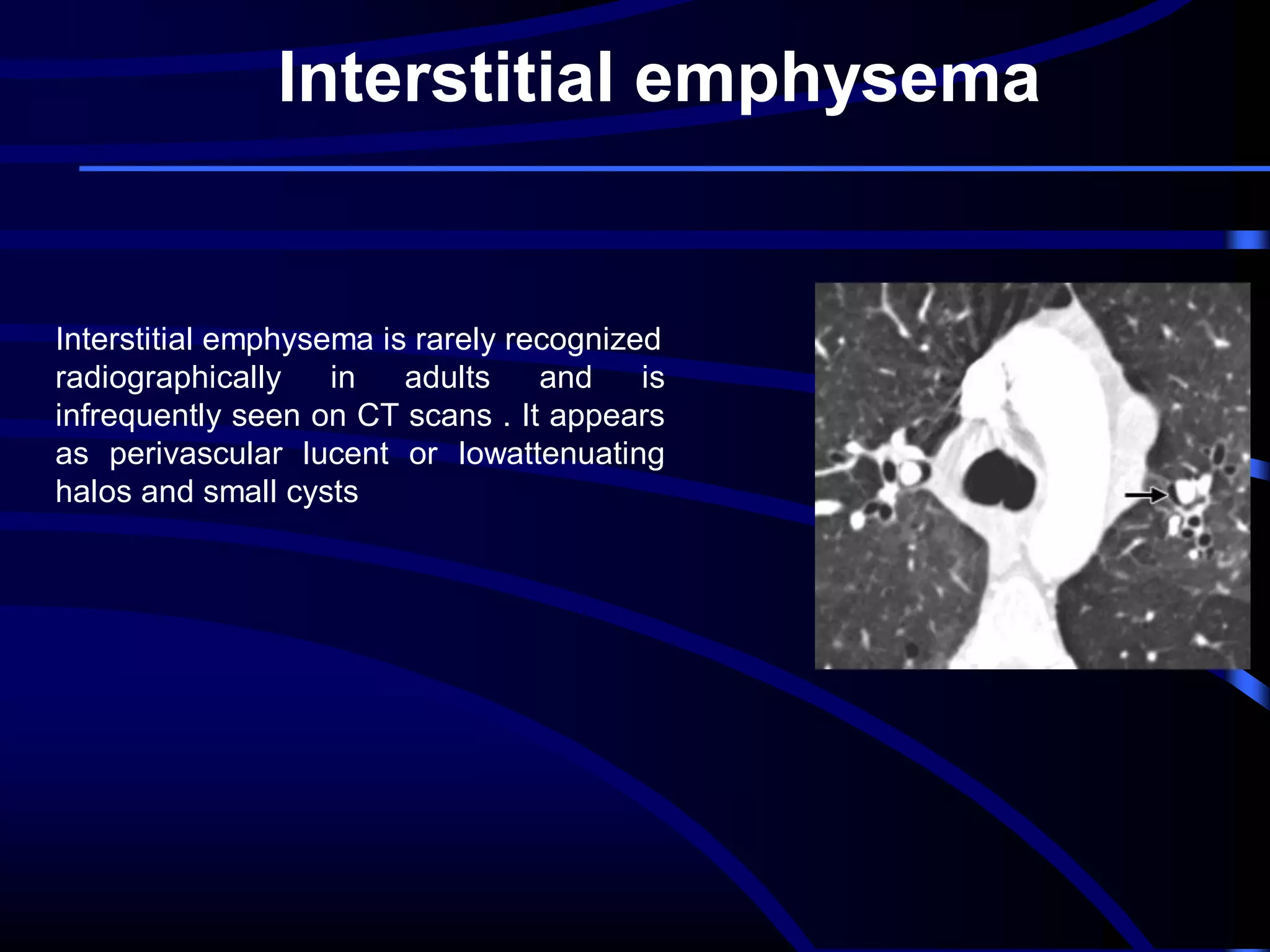
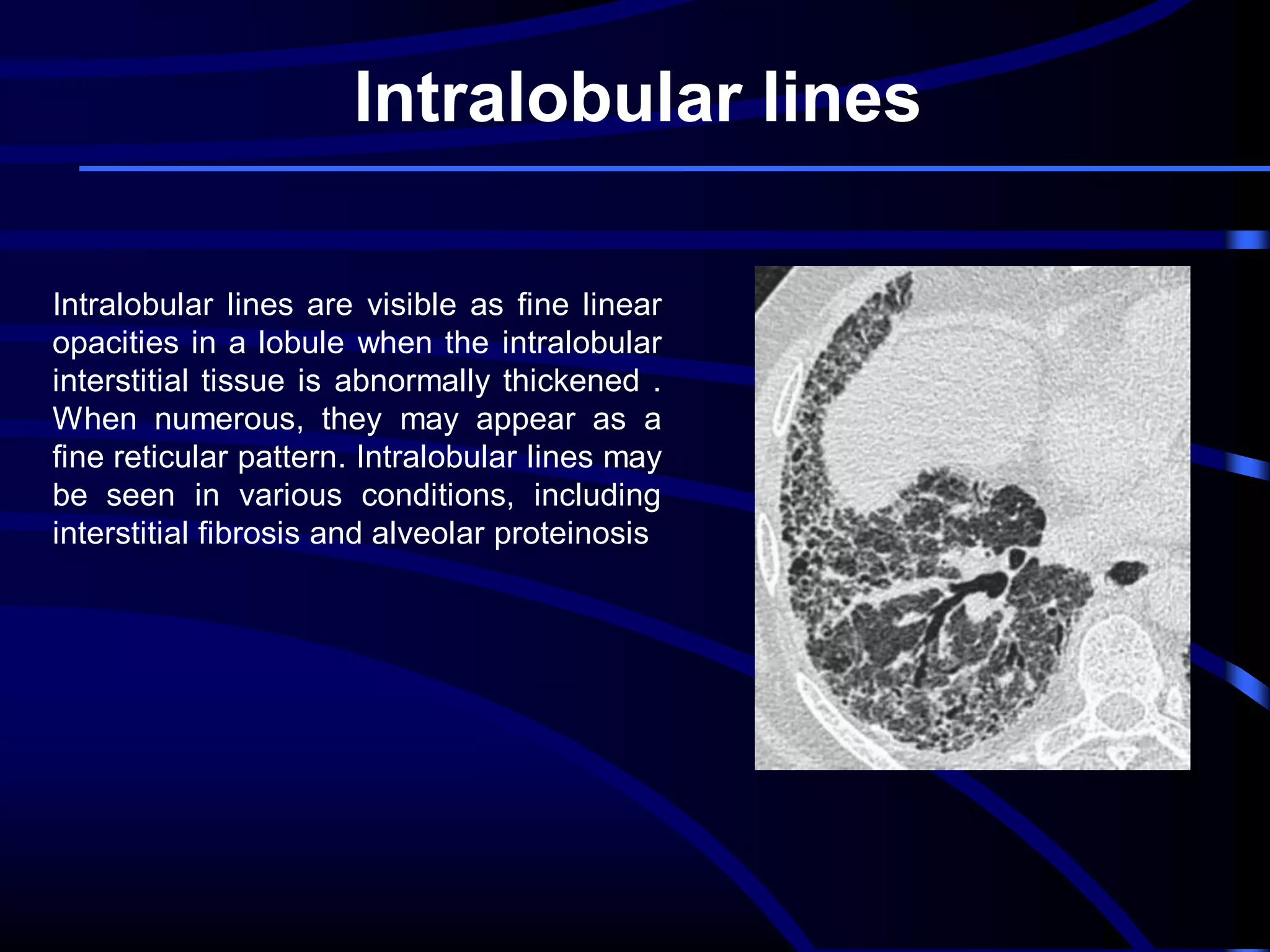
This document defines and describes various thoracic imaging terms related to the lungs. It discusses air bronchograms, air crescents, air trapping, and other terms. For each term, it provides a definition and brief explanation of what the term refers to in radiographic images of the lungs. The document is intended as a reference for radiologists and others to understand common findings seen in chest x-rays and CT scans related to lung pathology.