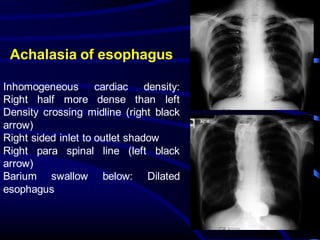
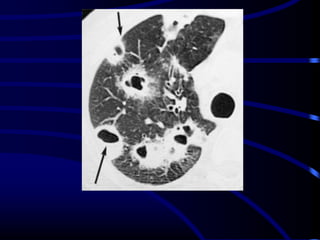
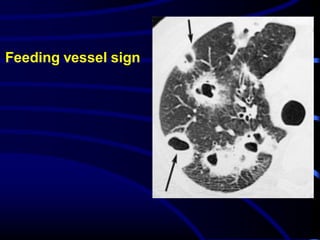
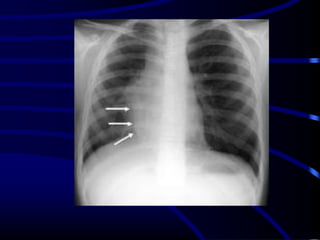
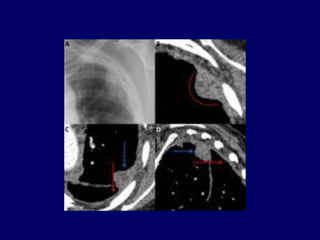
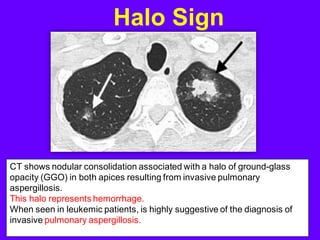
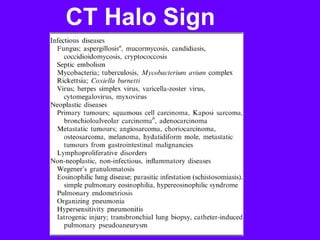
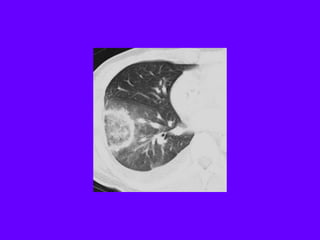
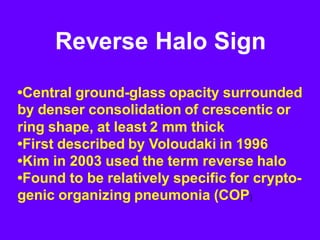
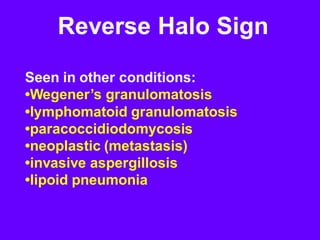
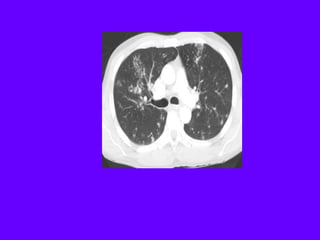
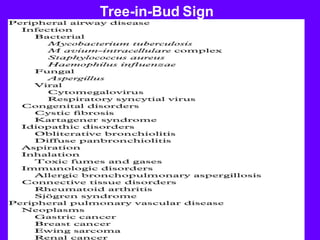
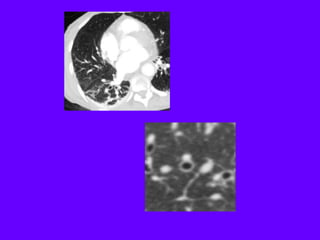
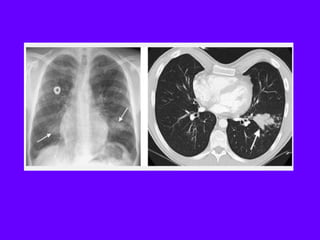
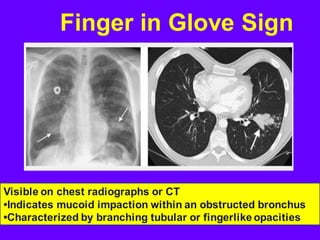
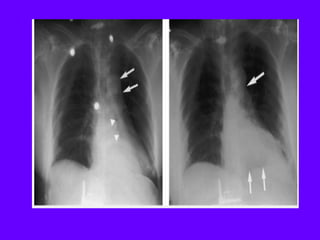
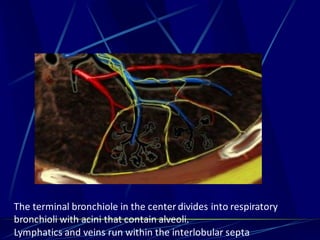
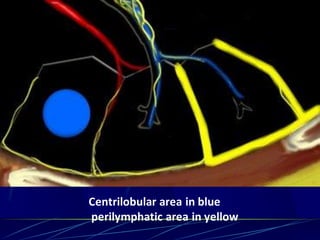
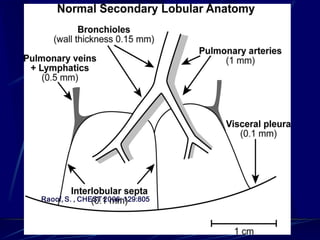
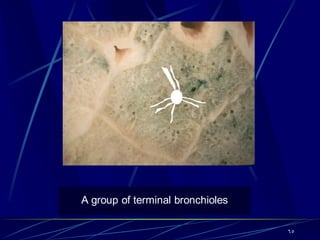
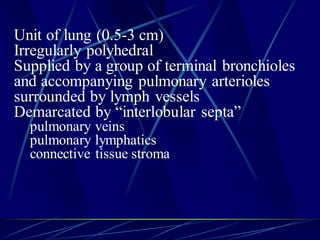
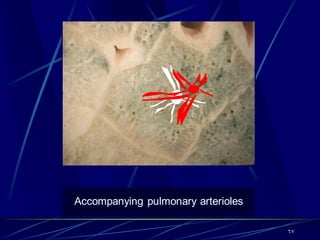
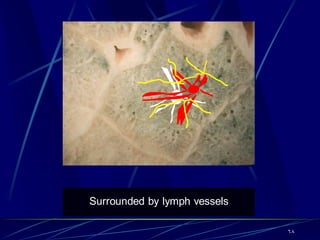
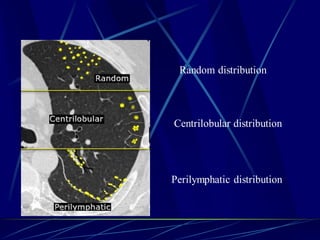
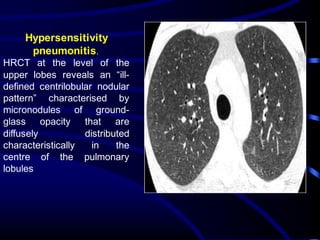
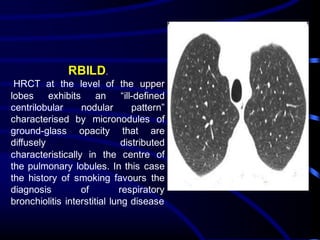
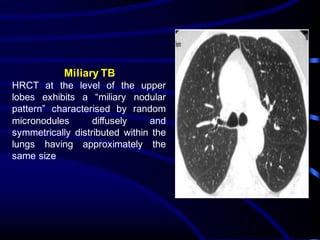
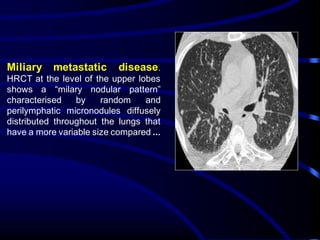
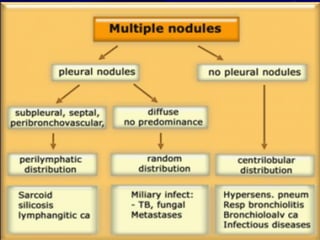
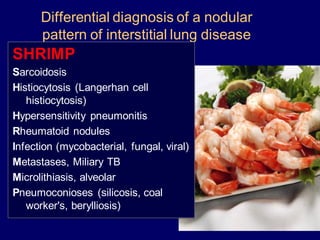
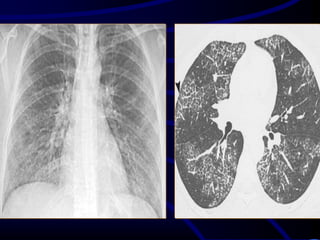
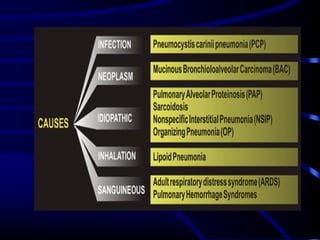
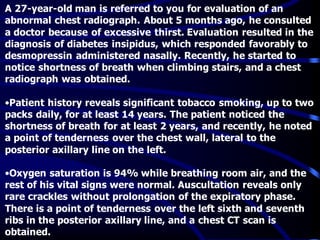
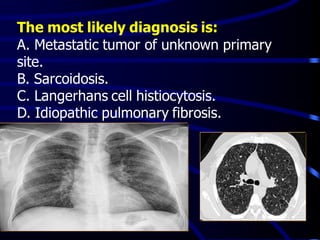
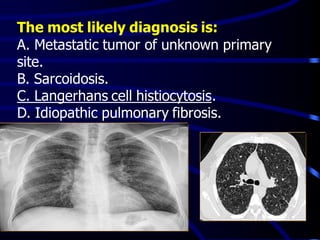
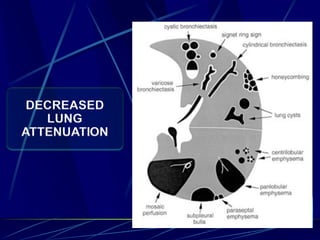
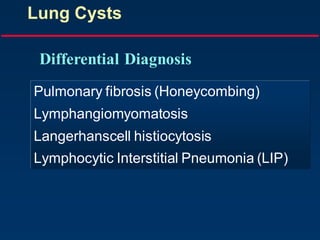
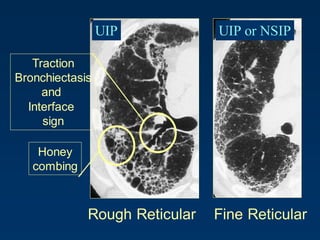
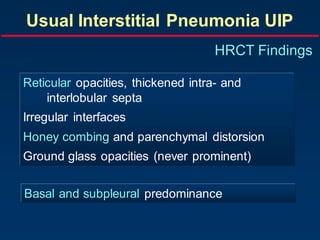
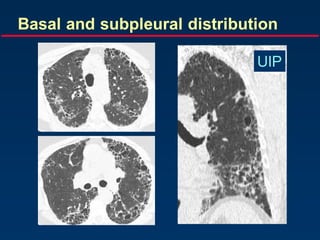
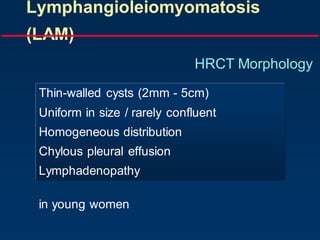
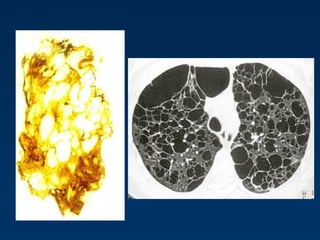
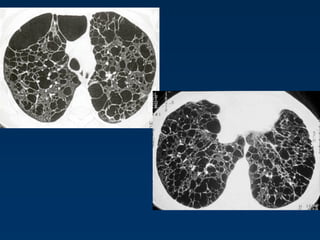
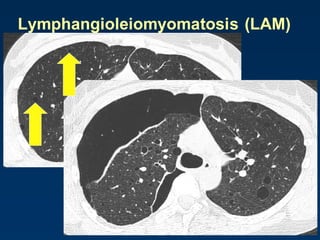
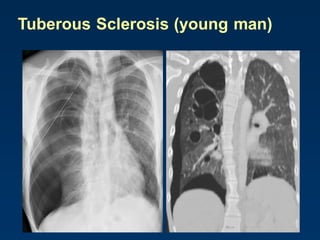
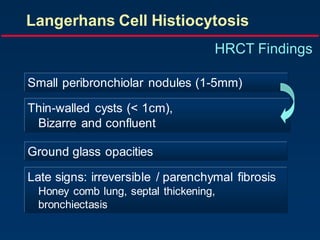
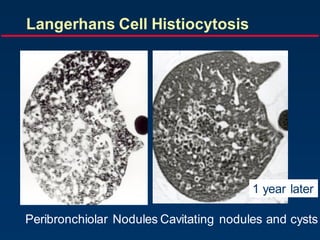
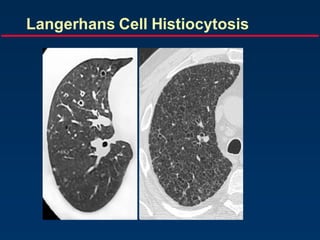
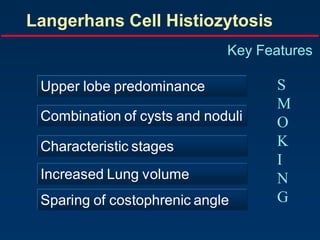
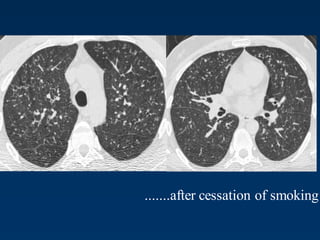
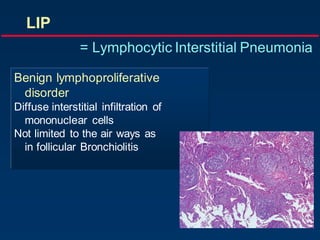
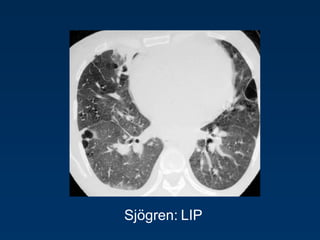
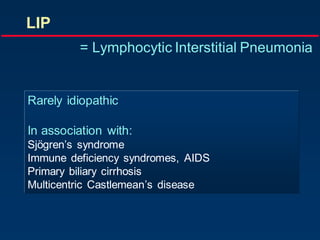
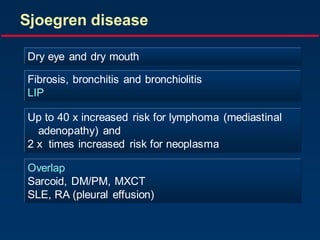
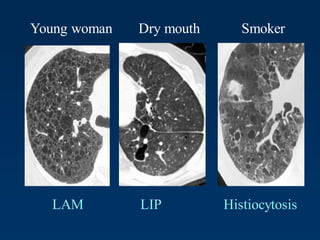
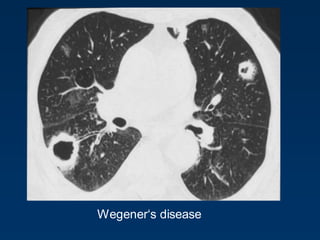
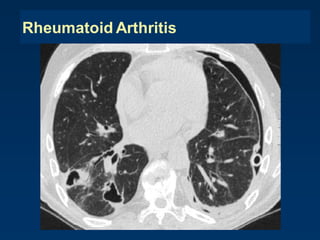
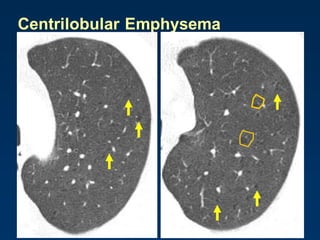
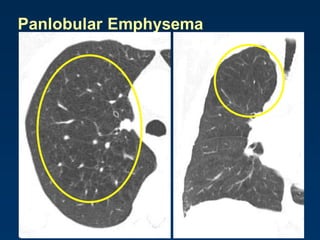
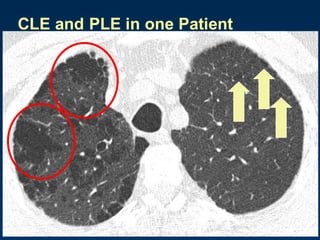
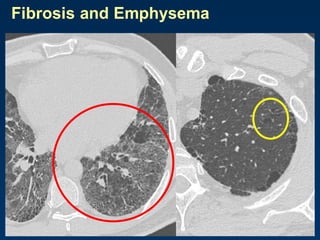
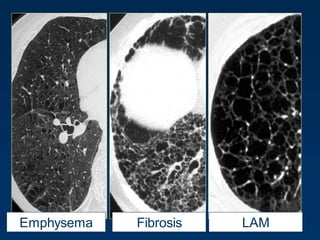
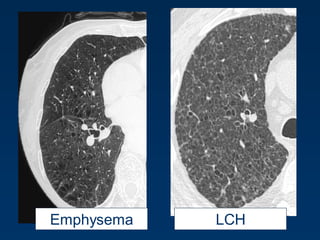
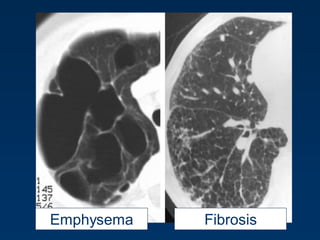
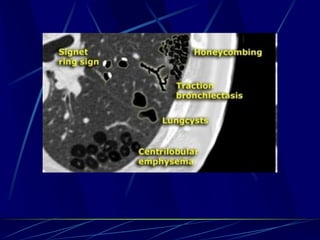
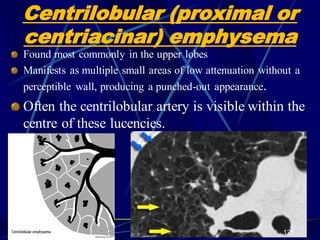
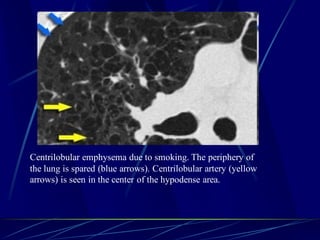
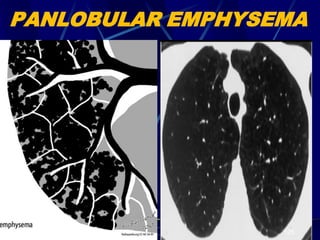
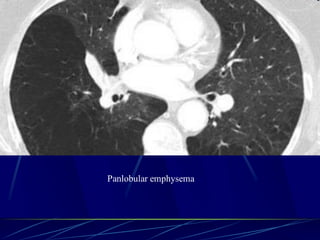
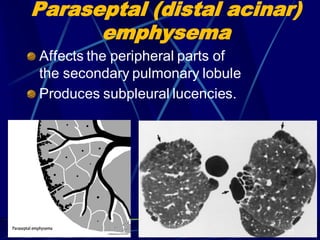
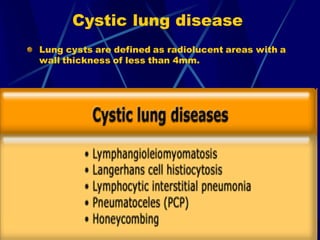
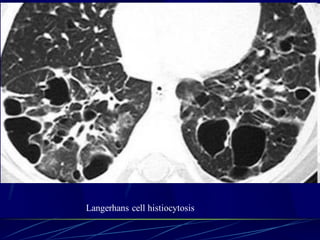
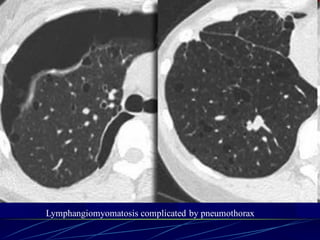
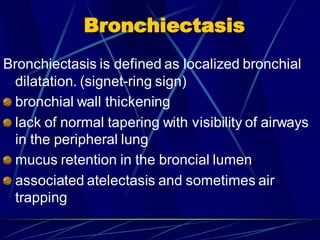
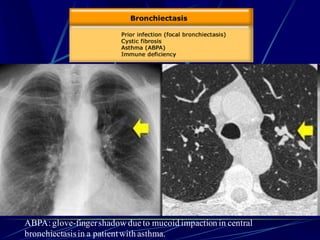
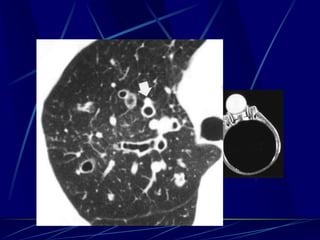
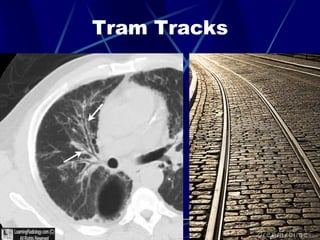
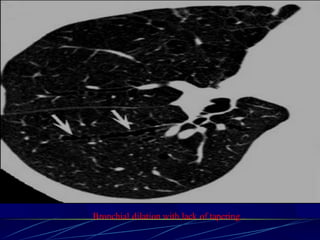
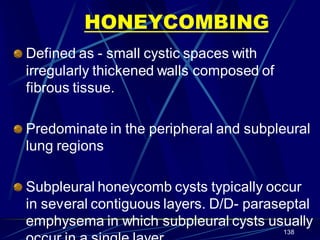
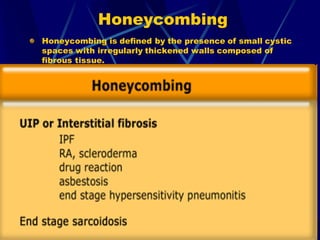
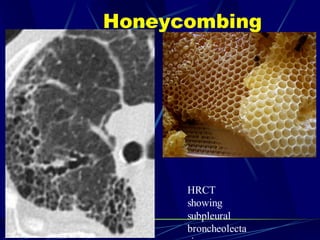
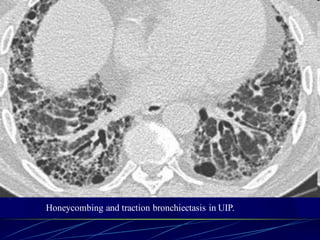
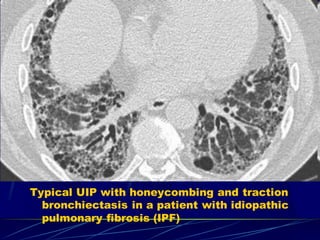
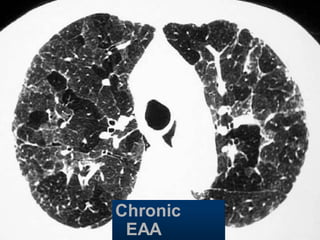
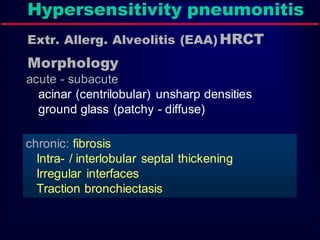
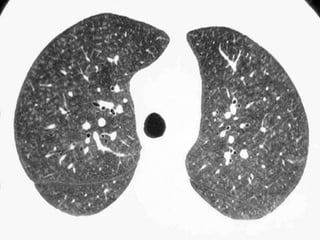
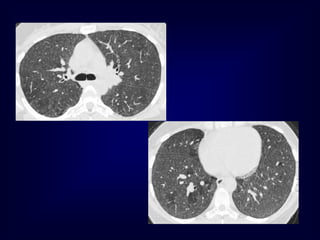
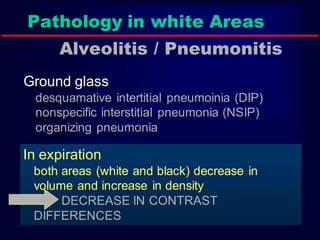
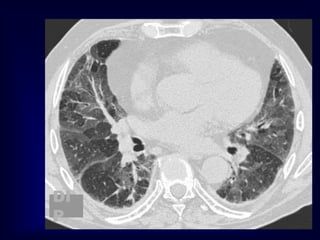
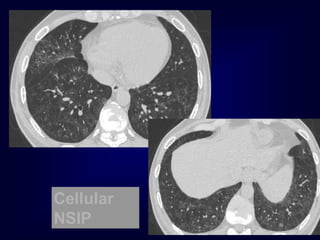
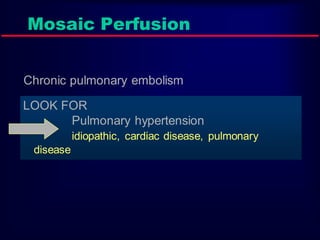
This document provides descriptions and radiographic signs of various pulmonary conditions seen on chest x-rays and CT scans. It includes definitions of terms like secondary lobule and centrilobular emphysema. Specific pathologies covered include Langerhans cell histiocytosis, lymphangioleiomyomatosis, pulmonary fibrosis patterns, and lymphocytic interstitial pneumonia. Radiographic findings are presented for different conditions along with accompanying CT images to illustrate signs like cysts, nodules, and reticulation. Differential diagnoses are discussed based on imaging appearance.